InvestingDoc
Personal Finance and Investing for Doctors


Financial Breakdown Of A Primary Care Clinic: How Much Money Does It Make
Today we are going to take a look at the financial breakdown of a primary care clinic that has recently opened. The numbers in this post are not my clinics financial numbers exactly. I don’t want to “dox” myself and I want to give anyone interested an idea of what is generally possible if you work hard. I’ve used the national average income for primary care physicians for gross revenue. The expenses are based on my expenses 6 months into being open. In some cases, I have rounded numbers to the nearest dollar amount for ease of reading. Keep in mind that this is a generalization. Costs may be slightly higher or income might be higher or lower.
Now, lets have some fun and look at the monthly financial breakdown of a primary care clinic.
Gross (Total) Revenue
This is the total amount of money that is brought into the clinic before any taxes, expenses, or deductions.
In order to understand gross revenue, we must first understand how doctors bill.
Doctors bill based off RVU’s, relative value units. Every service provided by a physician has a unique code and can be billed for. For example, smoking cessation counseling, time spent between 3-10 minutes: The code is 99406.
The government has assigned an RVU to each code. For example, a complex new outpatient visit is 3.17 work RVU’s or 2.38 RVU’s . There is a difference between (work RVU abbreviated wRVU) and (RVU). This will be outside the scope of this post, but if you want to know a bit more, here is a link to AAPC about RVUs. Basically, the larger RVU number includes facility fees, overhead, the work done, and total RVU also includes malpractice premium payments due to risk for each procedure.
Medicare on average pays about $66 per wRVU (in my area for 2019). The average primary care physician bills for about 5,000 RVU’s per year, which would equal about 7,000-8,000 wRVU per year. It’s unclear to me if these papers also count consumables such as vaccines in those RVU’s, which will add to the overall revenue.
To make numbers simple, lets say that the average primary care doctor bills for about $500,000 in insurance reimbursements per year. This is not an unreasonable amount at all for a full time primary care doctor who is seeing 15-25 patients a day. With this estimate our doctor is bringing in a gross revenue per month = $41,666.
Keep in mind this is an average number, work hard and you can increase the amount you’re bringing in each month.
Below are my average recurring expenses for the clinic at the six month point.
For my example, lets say as a new practice you decide to pay yourself $10,000 a month until you get a better sense financially of how things will go. This is exactly what I decided to do. I think this is a reasonable salary contribution for a start up medical practice. However, you might not take a salary for the first month or two after opening your practice ( I didn’t). As an owner, you will also be able to take distributions from the company in the form of dividends for any net income. I take these distributions quarterly.
It may be enticing to try to pay yourself totally in distributions to avoid paying payroll taxes, but this is something that will land you in trouble with the IRS. According to the IRS, you need to pay yourself a reasonable salary for your position worked. Reasonable is left up to interpretation and is based on many different factors. I am not a tax expert, so if you want to know exactly how you should pay yourself, then you should consult a local accountant. My accountant has told me not to even get close to the 50% salary, 50% dividends for payment structure. That for sure more than 50% should be taken as salary.
So, lets take a look at my average monthly bills for my first 6 months open.
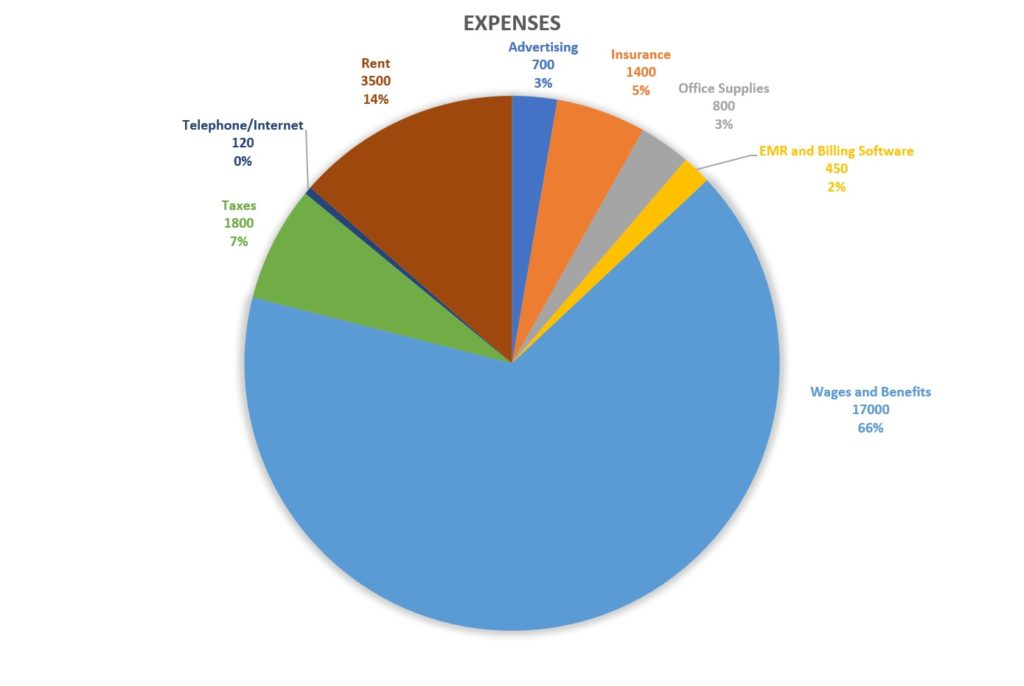
- Advertising: $700 (FYI: Now that I’ve maxed out my panel, I’ve stopped paid advertising)
- Insurance (This is not including health insurance for employees. This is Malpractice insurance cost, workers comp): $1,400
- Office Supplies $800
- EMR and Billing Software: $450
- Wages + benefits for employees: $17,000 (2 employees + Doctor)
- Taxes: $1,800 (As the employer you will have to contribute to taxes per employee paycheck. Social Security 6.2%, Medicare 1.45%)
- Telephone $120
- Rent: $3,500 (I share rent with another physician which is why it may appear low)
Total expenses: $25,870
Net Income:
The income left over after all expenses as above: $16,796
So, the doctor in this situation is getting paid $10,000 in salary and $16,796 available left over for distributions. This won’t fly with the IRS and I suspect will earn you a letter from them plus possible penalties trying to avoid paying payroll taxes. So, salary will have to be adjusted up and distributions will have to go down to avoid trouble with the IRS.
Total yearly gross salary for this primary care doctor who owns their own clinic is $321,552 per year.
Total overhead excluding the doctors salary: 36% in this example.
For those of you who do not think this is possible, my clinic continues to hover around 30% for my overhead (excluding physicians salary). We run lean, work hard, and overall love what we do. It was hard finding good help. I had to fire my first employee pretty quickly. However, despite all the negatives to running a business, this has been the most rewarding thing that I have ever done. If you choose to work more or less, you can make significantly more or less income accordingly.
The Drawbacks:
There are many drawbacks for the primary care clinic. Yes, the high potential salary is a blessing, but there area always drawbacks.
First, the doctor in this example is always on call, and if you averaged out pay per hour it wouldn’t be great compared to hospitalist work. I am on call 24/7, every holiday and every weekend while self employed. A huge drawback for many.
Second, there is a lot of stress to owning and running a medical practice. I have no business manager. This puts extra money in my pocket but extra work on my lap. If you are not the type of person who doesn’t mind writing an employee up for being late, working on payroll hours, or fixing a broken printer, then you won’t mind the job. There is a lot of bureaucratic paperwork that goes along with the job, like reporting to the state wages and paying payroll taxes quarterly. I have spent many hours after clinic on setting up the business of a primary care office.
Third, the stress of the unknown can get to you. Many sleepless nights were had when I started my practice. I was so worried no one would ever show up. I also was worried how things would go practicing solo, not having other doctors to bounce ideas off of if I had a question in clinic.
Finally, primary care is hard. If you want to open your own primary care clinic get ready. Primary care is very hard. Dealing with possibly 5+ chronic illnesses, worrying about preventative medicine, dealing with some demanding patients, and on top of that running a clinic can burn anyone out. You can easily get buried in paperwork and frustrated with patients who are angry with you. The job is already tough and adding another difficult factor to the job for most people seems to be a huge reason to avoid owning their own practice.
The Grass Can Always Appear Greener
It is not all roses, but I will say that demanding patients are everywhere. There are tough days, there are many more great days. Most of my patients are wonderful, kind, and want to get better. It is a blessing to have such potential high income in our profession. Overall, I wouldn’t change how things are going for any amount of money. I’ve built a steady panel of patients and things have become more on autopilot every day I show up to work. To all the people considering starting their own practice: The beginning is definitely the hardest. It gets so much better!
If you are even considering opening up your own practice, I say go for it!.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- ← How I Paid Off $150k In Loans In 1.5 Years
- Why Doctors Stay Employees Rather Than Owners →
You May Also Like

My Experience Using ZocDoc To Help Grow My Practice

More Details: How I Spent My Emergency Fund

The Benefits of Locum Tenens For Saving or Paying Down Debt
21 thoughts on “ financial breakdown of a primary care clinic: how much money does it make ”.
So now that you have filled your panel, any thought on adding a mid-level? Any chance you could do the financial breakdown for adding a PA/NP to a practice for those less informed of insurance and other considerations?
I will for sure be adding a mid level provider. I’ve already added a doctor and I am trying to hire another doctor so there will be 3 docs total. Once the doctors are up and running (they don’t have to have a full panel just the swing of things down in the practice) then I will bring on a PA or NP to my current clinic to cover me or the other docs when we are out.
From the glance of it, it looks like financially this is the most lucrative for owners of a medical clinic, not employing doctors. I started with physicians because when I’m off I don’t want to have to be asked medical questions and wanted someone who is completely capable of seeing all the patients and dealing with illnesses on their own independently. I’ve learned that starting up a business and running a business takes a lot of admin work and bringing on physicians allows me to take a step back every now and then and almost completely unplug.
I’ll absolutely post the financials as I go along though, even when I hire another doctor or NP.
Congrats on having a smooth running model! I hear that if you outsource billing, they take about 7% of the collections.. Did you include billers Payment in the employers list.. What EMR are you using now and do you like it. Did you take straight Medicaid when you started?
Hi, Thank you!
Billing companies I have found will take anywhere from 4-6%.
I have a biller in house so part of the overhead is collecting money and submitting bills.
I am currently using practice fusion.
I do not take straight medicaid. Where I am at, the fee schedule is so bad for medicaid that I wouldn’t even cover overhead with payments.
Thanks for checking out my website
Thanks for the reply!
Did you have any trouble contracting with the insurances.. like closed panels or capitations or holding you for too long?? If so, how did you manage.
I have a scenario where I’m independently credentialed but was contracted under a different employer tax ID. Now that I plan to establish my practice under my tax ID, I need to negotiate contracts with the insurances.. I’m trying to figure out if it will be to hard and if I have to take MSO or IPA help with contracting under their group rates, but there will be MSO restrictions..
I appreciate any input.. Thank you again!
Thanks for this encouragement. I am early into staring my own practice as a mid level for home care primary care and already exhausted… you have encouraged me today.
I’m happy to hear that I encouraged you! Best of luck on your endeavor!
This is great info. I’m an NP and have been open for 5 months and as of now I have about 850 patients. Looking at your numbers above, my question is: how did you do it with so few employees? I have myself, 2 MAs and my husband (he is an LPN up front to make appointments and also handles billing. I’m seeing about 15-18 patients per day. I will say, my MAs are great , but only one can draw labs. It puts a burden on us when someone needs to be off. We went through a few rough weeks also due to employee and child illness. I don’t want to burn out my assistants for sure, but also want to make sure that I do not become too top heavy. We did come from a corporate model where there was enough staff and the workload was not heavy. My patients are familiar with all of us as their care team. I am considering hiring someone else just so I can relieve myself of admin duties and my husband can mostly manage. The position would be part time at 24 hours per week. We also have 2 kids that are very active. Should I hire an additional person? I know we are going into sick season soon and I would expect to see at least 20 per day. Thanks for any advice!!
You need to automate. If you are solo, and you are seeing 18 pts a day, your check in forms, scheduling, everything should be automated. When I was running solo with 850 pts, I automated all of this. I also had an external biller while I was solo so I did not have to have them fully on staff since it would have been too much in payment for just one person bringing in the income. If blood draws are burdensome then send them to a lab nearby to get the blood drawn done. Push people to message in rather than call…that eats up a lot of time.
Do an audit of where you think everyone’s time is being spent and ask yourself is there a better way to accomplish this task. Instead of a patient spending 5 minutes on the phone trying to get insurnace information, send them a text, tell them to take a picture of it and text it back in. Lots of ways to be creative to get your employees off the phone and helping with seeing more patients more efficiently.
Very happy for your success! Everything is a journey and even though the initial phases were tough, look at you now! Congrats!
Thanks for the kind words! Have a good day.
Great job on getting your practice running! Overall, how quickly (months) did you fill up your panel?
I started totally from scratch and reached 5000 patients in my panel in about 18 months. That’s when I felt totally overwhelmed and stopped accepting new patients. Looking back I probably should have cut back earlier. However, I hired new doctors to join my group and they have been growing their practice.
Wow!!! Where was this?
I was subleasing from a surgeon. This is located in a major city in Texas.
Finding this post today has really lifted my spirits. I’ve always been so close to opening but then fear of the unknown gets the best of me. Also, did you take out a business loan to open or did you finance it yourself.
I financed everything myself by doing locums. The only exception is that I did take out a loan to buy the building that I am currently in.
This is great information and a great exercise for providers to gain an appreciation of a practice balance sheet. I helped my wife start her solo PCP practice 20 years ago with a few patient charts and a file cabinet. One note about the above numbers: Be sure to run them for the reimbursement AVAILABLE in your area. Most private PCPs in our area make their expenses on a capitated plan that new practices don’t have access to, so our revenue was all FFS—at about $60 a visit.
That number changes things, as a provider would need to see about 35 patients a day for 20 days a month just to break even on the above expenses, which is almost double the above patient visits a day.
It is great to see a provider sharing information to help others. I have been amazed at how little sharing exists in practice management among providers.
Thank you for sharing your experience! I’m sure many will find it very helpful. As for expenses, it seems like you didn’t mention anything about medical equipment. I’m really wondering how much money it might take to buy equipment. They say that it’s extremely expensive.
What type of medical equipment? Yes, some things are very expensive. Exam tables are about $1000 – $1500 each. Computers about $1,000 each. We paid about $300 for our EKG machines each. Yes, you can spend a lot of money on equiptment if you are going to need surgical supplies or asthetics devices.
I appreciate this essay. I am also considering private practice, and there doesn’t seem to be enough guidance these days as most, if not all, of my colleagues are employed by a big hospital. There is more doom and gloom about decreasing reimbursements and increasing administrative headaches imposed by CMS, than the upside. It’s nice to hear encouragement from another doctor for a change. I just found your blog, and look forward to learning more !
Leave a Reply Cancel reply

Home Articles ROI Revenue Per Visitor: Definition, Formula & Best Practices
Revenue Per Visitor: Definition, Formula & Best Practices

Anthony Brebion
Revenue Per Visitor, or RPV, is a highly effective way to measure how your online sales are performing. With so many metrics available to businesses, it is one of the most comprehensive available, covering the myriad of blind spots that are inherent in many other data metrics.
What Is Revenue Per Visitor?
Revenue Per Visitor is a way to accurately assess average revenue per visitor to your website.
The calculation is made by dividing the total income by the number of visitors during a specific time period . For example, if your income for January to March is $20,000, during which time you attracted 5,000 visitors, then your RPV would be $4.
RPV works differently from Conversion Rate (CVR), although it is a similar metric using some of the same data. As we will see, CVR is not as accurate as RPV , and can lead a business down something of a blind alley and affect both website design and marketing campaigns.
Why Use Unique Visitors?
Revenue Per Visitor does not use the total number of visitors to your site in its calculations. Instead, it counts only unique visitors, with each individual counting as just one visitor. In other words, visitors, not visits. This is because almost all first-time visitors to a site, more than 99%, will not make a purchase . Typically they might want to compare prices or offers on another site, or perhaps they want to mull things over before making a purchase, particularly if it’s an expensive one.
This can skew the results considerably and provide falsely negative data on how much a company will earn per visitor. On the other hand, if you are gaining a lot of recurring buyers, you may wish to document this trend and use total buyers instead. This might depend on what it is you are selling, as well as whether you want to track individual habits as well as revenue.
Why Use Revenue Per Visitor?
RPV is a much more thorough and insightful metric for those who wish to measure online sales than Conversion Rate (CVR).
In fact, many of the metrics used in e-commerce have enormous blind spots that can lead you to make poor decisions made with accurate, but incomplete, data.
Put simply, conversion rate tracks the percentage of visitors to your site that makes a purchase. If the product or products you are selling are of one price, this would paint a complete picture of how your business is performing. Most e-commerce platforms, however, are selling products of different value. For example, a conversion rate of 3% for a fidget spinner worth $2 is very poor, but for a sofa worth $1,000 it is highly desirable. So what is needed is a metric that takes into account AOV – Average Order Value.
The average order value is the average revenue made per visitor . The aforementioned fidget spinner has an AOV of just 6p, but the sofa has an AOV of $30. So why not use this metric to calculate how much a business earns per visitor? Well just because conversion rate comes with an inherent blind spot, doesn’t mean it’s a metric without merit. If the only data you have is AOV, how are you to know if your website is performing to its full potential? Also, a low conversion rate directly affects your website’s ranking. The lower the ranking, the less likely customers are going to find it in the first place. The answer? Combine both metrics. This is how RPV came into being.
How To Improve Revenue Per Visitor
There are many methods and ideas that help improve a business’s average revenue per customer, but each tip should not automatically be considered a one size fits all deal. In fact, a lower RPV is not always a sign of a poorly performing website. For example, high traffic that garners low sales, and therefore a low RPV, can lead to higher sales over an extended period of time. It is therefore often good practice to keep every metric in proportion to other data.
Having said that, there is a little doubt about the power and insight that revenue per visitor can provide. These include:
Recommendations
Reward programs.
- Basket reminders
Optimization
A tried and tested method of commerce since humans began trading, upselling is the method of suggesting upgrades or add-ons to the original purchase . For example, a tech salesperson might suggest that spending an extra $50 would result in a faster processor, meaning the laptop will avoid becoming obsolete in the near future. Or perhaps the next model up, which is only $70 more, has a free upgrade for the latest operating system.
Upselling is a balance, one where it is important to make the customer feel as if they are getting something of worth, or perhaps that it would be foolish not to when spending that little bit more. According to a study from Predictive Intent, upselling increases sales by over 4% for e-commerce businesses, and is twenty times more likely to be effective than non-complimentary recommendations.
Despite what was said in the previous paragraph, recommendations can be a highly effective way to increase revenue. By simply suggesting other items, there is little doubt that basket totals increase. By how much will depend on the effectiveness of the recommendation engine. This can be tricky for small businesses with little or no data on their customers, the more information you have, the better recommendations work , but some common sense can work wonders here.
For example, complimentary suggestions, those related to the purchase, will likely result in higher purchase totals. If someone buys a laptop, suggesting a wireless mouse or external hard drive will likely be yield better results than stereo equipment.
It is hard enough finding customers in the first place, when you have their attention, creating an experience and incentives for them to return is essential. Reward programs are perfectly designed to achieve this.
Much like supermarket reward points, these systems encourage customers to return to an e-commerce website, rather than a rival business, by making it worthwhile for them to do so. Reward points are just one method of encouraging loyalty, however. Exclusive offers for returning customers have proven to be highly effective when implemented in the right way. This can be particularly useful during the Christmas period when businesses are most likely to encounter new customers.
Basket Reminders
Revenue per visit can be greatly reduced by those abandoning their purchase halfway through the process . Some estimates have the rate of abandonment at almost 70%. There are many reasons why this might happen, and some, such as the process taking too long, can be dealt with by redesigning parts of the website. Whatever the reason, it is possible to turn some of those near misses into hits.
Simple apps and email campaigns can target those easily distracted customers into big spenders, and such solutions are highly cost-effective. What’s more, setting up such apps and campaigns take the minimum of effort and can lead to loyal customers that make regular purchases.
Depending on the size of a business, setting up a live chat feature can increase revenue in some surprising ways. Firstly, customers are more trustful of a website that has an easy to use customer service platform, and live chat is the most convenient online source.
Secondly, particularly if it’s a major purchase, many customers seek reassurance or extra information about a product. Such reassurance not only makes it more likely a sale will occur, but that returns and unsatisfactory experiences can be greatly reduced.
There is also the opportunity for additional revenue from upselling or special offers to be presented to the customer, one to one. Don’t forget as well to A/B test your live chat solution. You may be surprised!
Website optimization is key to best practices in e-commerce and is the most thorough and data-driven aspect of understanding how well a website is performing. This might include heat maps, where businesses can see which part of a page’s content has been engaged with most or testing different versions of a website to ascertain which setups work best. This is known as A/B testing.
Optimization provides data beyond simple metrics and allows a business to make sense of the data at a much more profound level, putting into context what might otherwise be cold, hard numbers that lack context.
Calculating Year Over Year Revenue
Site revenue is pretty straightforward to calculate over the course of a single year. For example, in 2014 Business A’s revenue was $200, in 2015 it was $250. Subtract the $200 from the $250, leaving $50. Then divide the increased total by the original figure from 2014 (50 divided by 200), equalling 0.25. Lastly multiply that by 100, giving you the figure of 25% growth.
For year on year calculations you will need to use Excel, so as you might imagine, it isn’t so straightforward. This method works for any growth calculation beyond one year.
To calculate overall growth, from 2014 to 2016, simply use the formula above, but the calculating year on year requires three steps. First using the year ending figures for 2016, divide it by the yearly figures for 2014 (350 divided by 200 = 1.75).
You might also like...

Subscribe to our Newsletter
AB Tasty's Privacy Policy is available here .
We use third-party analytics cookies to understand how you use our website so we can build better products.
Revenue per Visitor (RPV)
Measure the total amount of revenue generated by a single visit to your site.
Track all your Ecommerce KPIs in one place
Sign up for a 14-day free trial and start making decisions for your business with confidence.
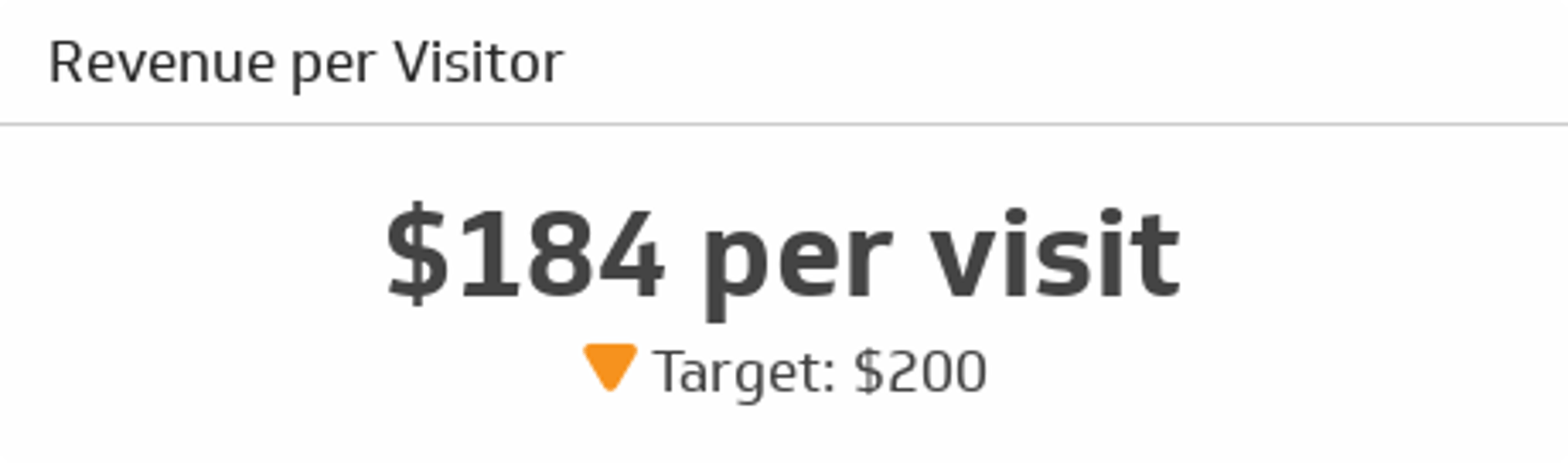
The Revenue per Visitor metric lets you track the total amount of revenue generated per single visit to your online store.
Regularly monitoring the "Revenue per Visitor" e-commerce metric helps businesses understand the value of each visitor, measure the success of marketing efforts, and make data-driven decisions to optimize the user experience, product offerings, and sales strategies to maximize revenue generation.
(Revenue generated by visitor A + Revenue generated by visitor B +...+ Revenue generated by visitor N)/Total number of visitors
Reporting frequency
Example of kpi target.
$200 per visitor
Store Owner, Online Sales Manager
Related Metrics & KPIs
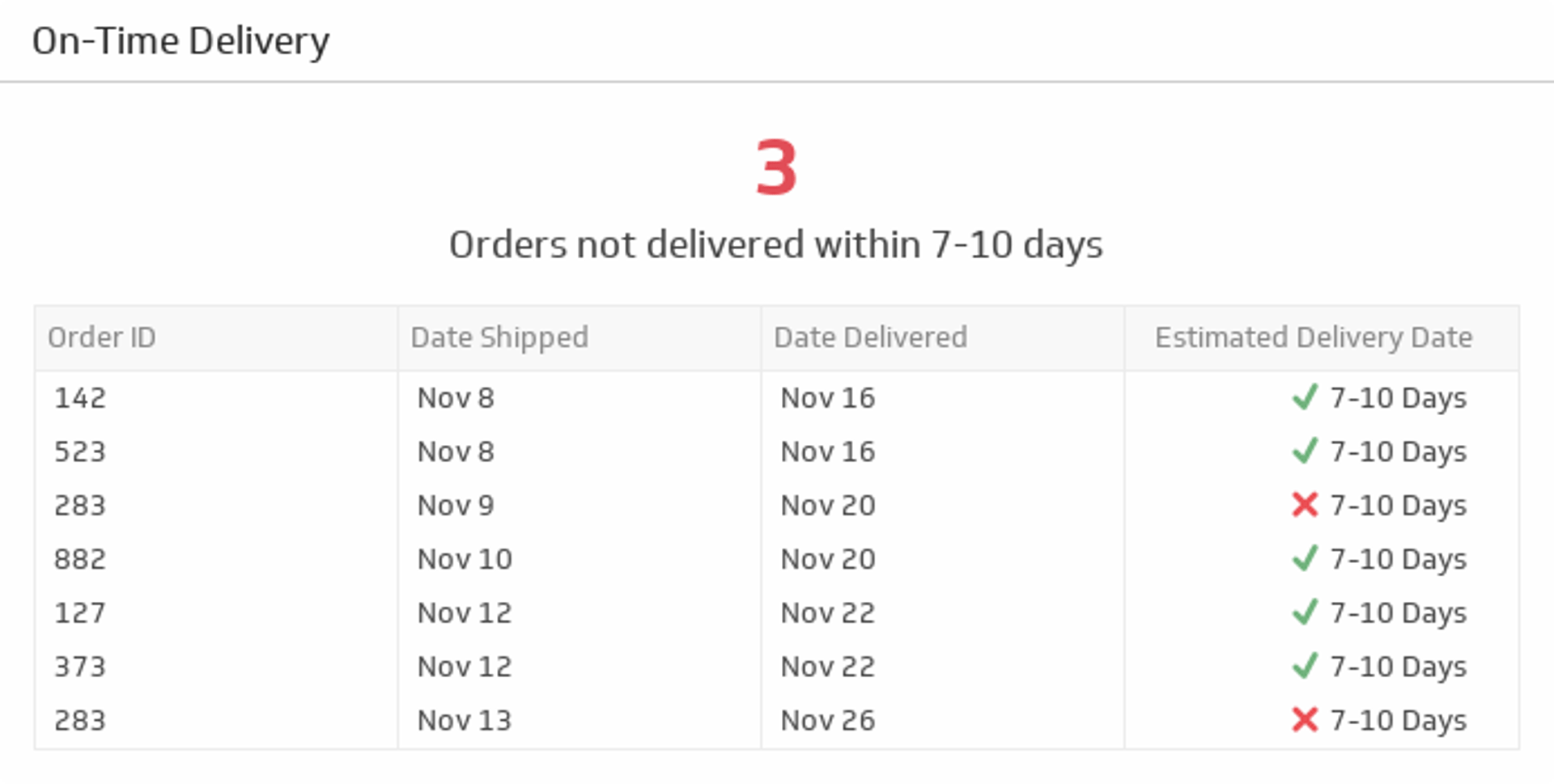
On-Time Delivery
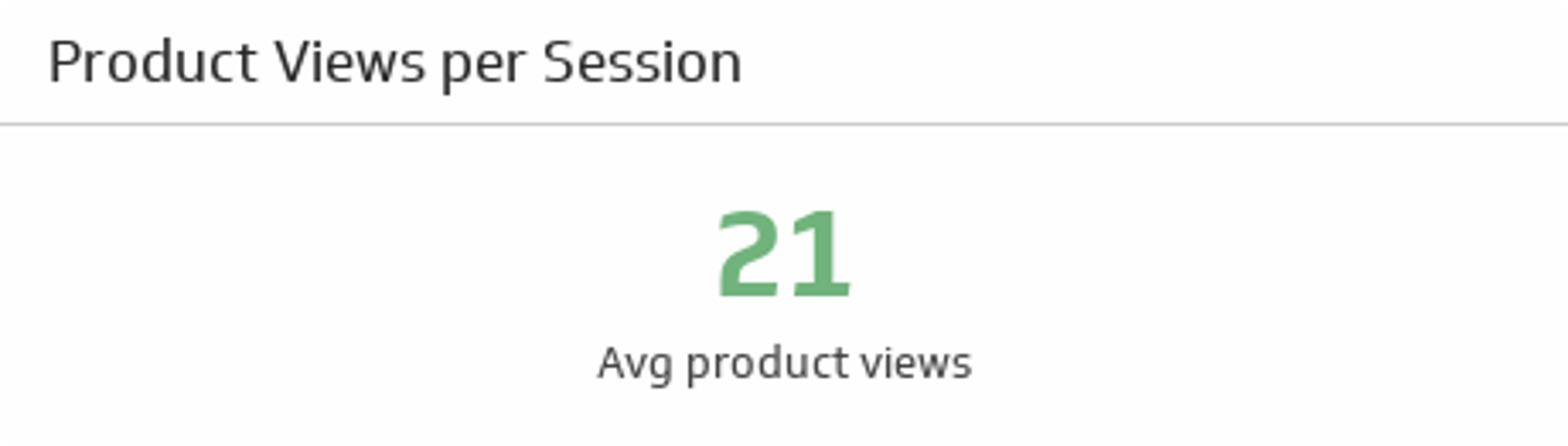
Product Views per Session
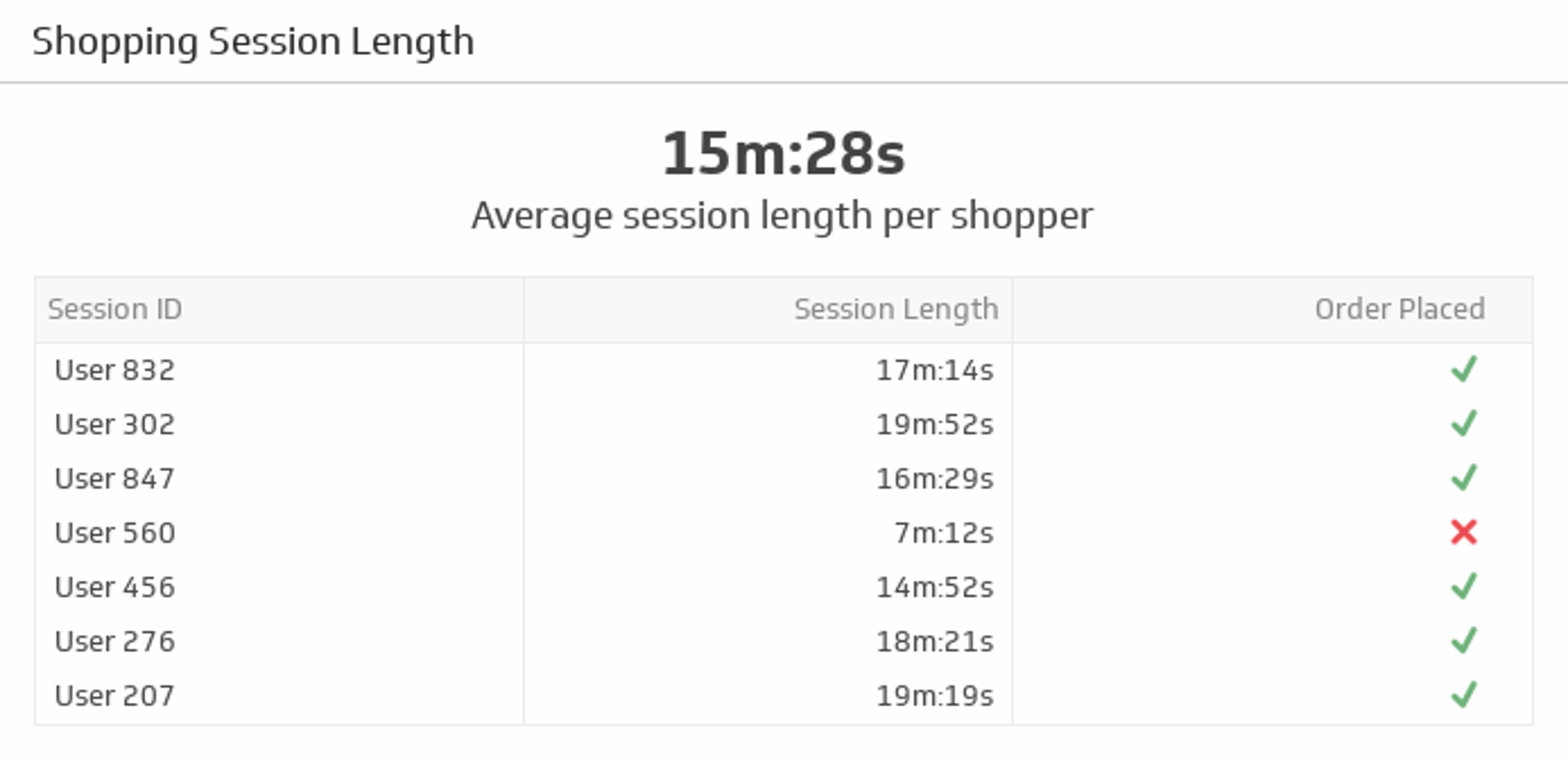
Shopping Session Length
Start tracking your metrics Level up your analytics with Klips.
- Metric Library
- Integrations
- Google Universal Analytics
Revenue per Visit

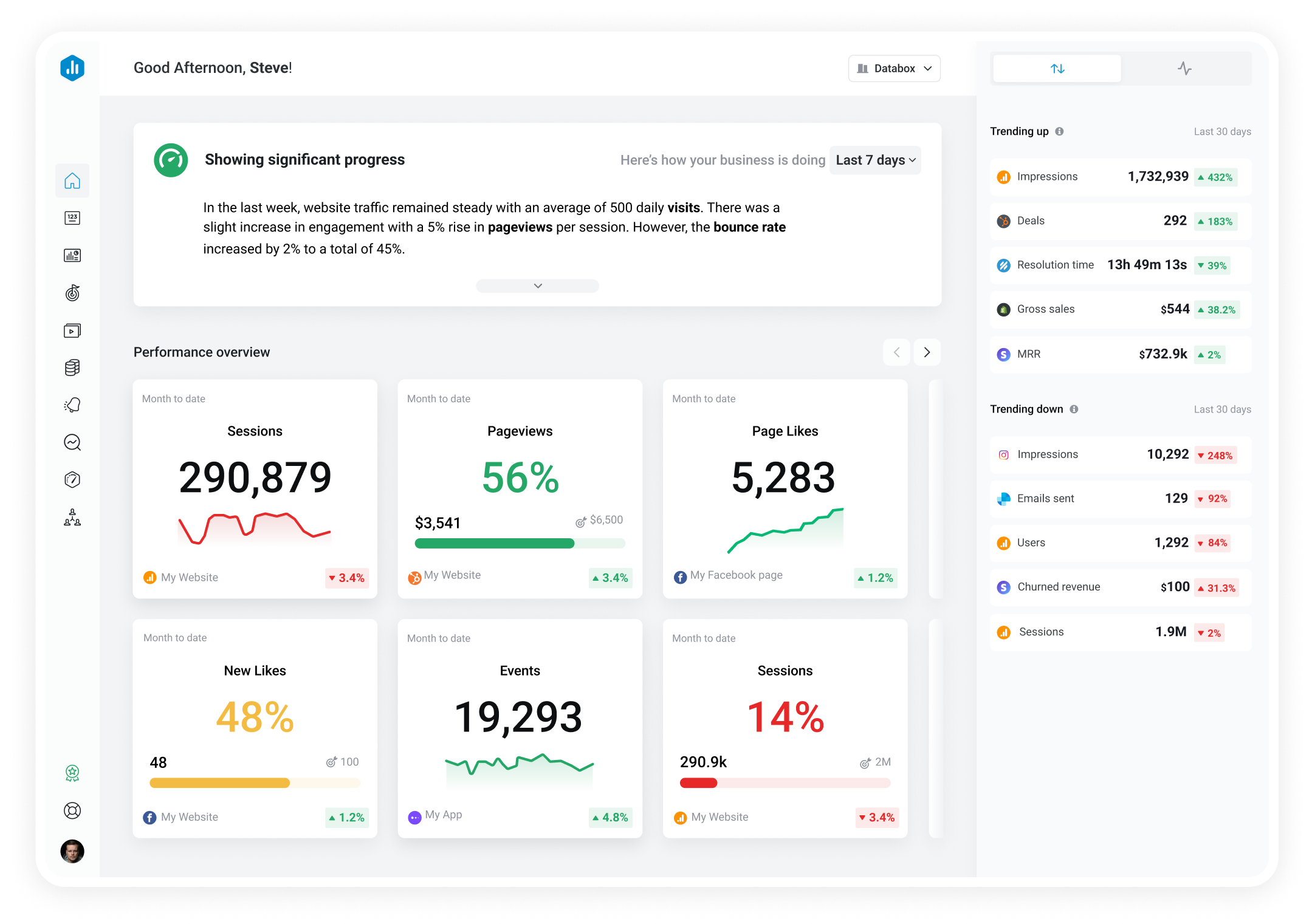
Revenue per Visit is a metric that calculates the average amount of revenue generated during a website visit. It helps to measure the effectiveness of marketing efforts, and provides insights into the purchasing behavior of visitors.
With Databox you can track all your metrics from various data sources in one place .

- Tech details
Visualizations

Used to show a simple Metric or to draw attention to one key number.
How to track Revenue per Visit in Databox?
Databox is a business analytics software that allows you to track and visualize your most important metrics from any data source in one centralized platform.
To track Revenue per Visit using Databox, follow these steps:
- 1 Connect Google Universal Analytics that contains the metric you want to track
- 2 Select the metric you want to track from the list of available metrics
- 3 Drag and drop the selected metric onto your dashboard
- 4 Watch your dashboard populate in seconds
- 5 Put Revenue per Visit on the Performance screen
- 6 Get Revenue per Visit performance daily with Scorecards or as a weekly digest
- 7 Set Goals to track and improve performance of Revenue per Visit

Set Goals to track and improve your performance

Get your daily progress every morning with Scorecards

Receive detailed weekly performance updates

Built your own custom metrics with Metric Builder

Get instant insights into your top-performing metrics
Google Universal Analytics Revenue per Visit included in Dashboard Templates 2
Google universal analytics (ecommerce overview).
Google Analytics dashboard template which will give you insights about your Transactions and Revenue, conversion rates and more.

Conversion & Loyalty Analytics
This template offers overall sales insights with a focus primarily around returning customers to gauge brand loyalty.

- Description Revenue per Visit is a metric that calculates the average amount of revenue generated during a website visit. It helps to measure the effectiveness of marketing efforts, and provides insights into the purchasing behavior of visitors.
- Category Website Analytics
- Subcategory Revenue
- Date Added 2015-04-28
- Default Format PrefixCurrency
- Cumulative Support No
- Favorable Trend increasing
- Changing historical data No
- Forecast Support Yes
- Benchmark Support Yes
- Dimension N/A
- Metric Type general Learn more
- API Value Key
- API Dimension Key
- API Endpoint https://analyticsreporting.googleapis.com/v4/reports:batchGet
Related Metrics
Sessions by landing page.
Sessions by Landing Page is a metric that shows the number of sessions (or visits) that started on a particular page of a website. It helps evaluate the effectiveness of different landing pages in attracting and engaging visitors.
Sessions by New vs Returning
This metric measures the number of sessions by users who are visiting the website for the first time (new) as well as those who have visited before (returning). It provides insights into user behavior and helps target marketing efforts towards each group.
Bounce Rate
Bounce rate is a metric that measures the percentage of visitors who leave a website after visiting only one page. A high bounce rate is often an indicator of poor website user experience or irrelevant content.
Goal Conversion Rate by Channel
The Goal Conversion Rate by Channel metric in Google Analytics measures the percentage of website visitors who completed a specific goal (such as making a purchase or filling out a form) divided by the total number of visitors coming from each marketing channel (such as organic search, social media, or email). This helps identify which channels are driving the most valuable traffic and conversions to your site.
Transactions
The Transactions metric in Google Analytics tracks the number of completed purchases made on an e-commerce website, providing valuable insights into the website's revenue and conversion rates.
Avg. Revenue per User
The Avg. Revenue per User metric measures the average amount of revenue generated per user on a website or app, providing insights into the overall profitability of the user base.
Screen View by Screen Name
Screen View by Screen Name is a Google Analytics metric that tracks the number of times each screen or page of an app or website is viewed by users, identifying the screens by name to allow for easy analysis.
Screens / Session
Screens / Session is a metric that shows how many screens a user views before leaving a website or app. It provides insights into user engagement and can help identify potential areas for improvement in app or website design.
Track all of your key business metrics from one screen
Build your first dashboard in 5 minutes or less
Latest from our blog
- New in Databox: Analyze The Performance of Any Metric or KPI With Metric Insights April 22, 2024
- The Benefits of Hiring a Fractional Chief Marketing Officer (fCMO): Perspectives of Agencies, Buyers, and fCMOs April 18, 2024
- Metrics & KPIs
- vs. Tableau
- vs. Looker Studio
- vs. Klipfolio
- vs. Power BI
- vs. Whatagraph
- vs. AgencyAnalytics
- Product & Engineering
- Inside Databox
- Terms of Service
- Privacy Policy
- Talent Resources
- We're Hiring!
- Help Center
- API Documentation
The Financial Metrics that Matter Most to Therapy Private Practices
These numbers that could mean the difference between growing your practice and shuttering your doors. Click here to learn more.

Get the latest news and tips directly in your inbox by subscribing to our monthly newsletter
According to Pink Floyd, money is a “gas.” While the surface level interpretation of that lyric may be that money is fun and entertaining, the word “gas” seems deliberate here. After all, money is fuel. We as a society run on it, and yet, so many of us—including rehab therapy professionals—manage it poorly. The trick to better financial management is knowing what to actually manage—or more specifically, what to track, monitor, and act upon. With that in mind, here are the financial metrics that matter most to rehab therapy practices:
Days in A/R
Cash is king, so the sooner you can convert revenue into cash, the better. But, in between funds promised and cash-in-hand lies accounts receivable (A/R)—that awkward middle stage where your business eagerly awaits payment.
Days in A/R is defined as the number of days it takes for your clinic to get paid. Here’s how to calculate this number (according to AAFP ):
- Add all of the charges posted for a given period (e.g., 3, 6, or 12 months).
- Subtract all credits received from the total number of charges. (That way, you don’t get an overly positive impression of your practice.)
- Divide the total charges, less credits received, by the total number of days in the selected period (e.g., 30 days, 90 days, 120 days, and so on).
- Divide the total receivables by the average daily charges.
Everyone wants money in the bank faster, so once you know your average days in A/R, look for ways to shave time. For example:
- Pinpoint those slow-to-pay payers, and address payment come contract time.
- Collect copayment upfront, and scrutinize your invoicing and collections practices.
- Offer early payment discounts.
- Allow for payment plans. But, as AAFP advises, “Payment plans that extend the time patients have to pay accounts can result in an increase in days in A/R. Consider creating a separate account that includes all patients on payment plans and determine whether your practice should or should not include this ‘payer’ in the calculation of days in A/R.”
- Account for 90-day and 120-day buckets. “Good overall days in A/R can also mask elevated amounts in older receivables, and therefore it is important to use the ‘A/R greater than 120 days’ benchmark,” explains AAFP.
Collections
Expected vs. actual.
Most clinics track net revenue per month and per visit , but you can take this a step further by narrowing your focus to reimbursements specifically and comparing expectation to reality. According to this article, expected collection “is the payment amount the...practice expects to receive for a given service based on the contract between the practice and the insurance payer.” Chances are pretty high that the actual reimbursement amount will differ from the expected amount, but tracking this disparity 1.) enables you to track cash flow, and 2.) alerts you to potential collection issues. Often, the discrepancy will be the result of reduced or denied payments. And there are fixes for those . But, you can’t fix what you don’t know is broken, so regularly compare expected vs. actual reimbursement per visit and segment by therapists and payers.
Copay Collection Percentage
Not to sound like a broken record, but it’s imperative that you collect copays upfront whenever possible. We’ve all seen the stats: chances of collection decrease by 20% after the patient leaves the office. So, institute a check-in process that includes copay collection and then hold your front office staff accountable by monitoring your copayment collection rate.
First-Pass Acceptance Rate
Want to know how accurate or clean your claims are? Want to know if your payer processes are in good shape? Then measure how many of your billed services were paid on the first attempt. Low first-pass acceptance rates are indicative of a much larger problem, and to paraphrase denial management expert—and special guest on our Down with Denials webinar—Diane McCutcheon, you've got to identify the problem in order to stop the bleeding.
Productivity
Revenue per therapist.
To truly measure your providers’ productivity, go beyond the basic metric of number of patients per therapist per day. As this article points out, “For a true measure of productivity, you must consider the average amount of revenue each therapist is generating—per month, per day, or even per visit.” This enables you to monitor time management and accurate billing.
Units per Hour per Therapist
Time is money, so it’s important to examine the number of units your providers are billing per hour. In addition to uncovering instances of over- or under-billing, you can also determine if your front office is underbooking.
Gross Margin
“Gross margin tells you how much is left after paying for the people and things that generate that revenue (i.e., the ‘cost of revenue’),” Jacob Findlay, Fullbay founder and CEO (and former WebPT director of finance), explains in this post. To calculate this number, subtract the cost of your therapists, assistants, therapy supplies, and anything else directly tied to actually providing therapy treatment from your total monthly revenue.
Operating Expense
Operating expense is the cost of overhead. You can determine this by adding together the costs of rent, advertising, office staff, non-therapy supplies, and anything else that’s not directly related to therapy services. “You can choose to allocate a percentage of rent to gross margin or simply count it all as overhead,” explains Findlay.
To quote Pink Floyd again, “Grab that cash with both hands and make a stash.” Your stash is your net income, or “what you have left after paying for the cost of revenue and overhead,” says Findlay. Essentially, this is what goes into the practice owner’s pocket—or more accurately, bank account—when all's said and done. And you absolutely want money in the bank if you want to not only stay open, but succeed. As Findlay explains, “no matter how dedicated you are to making a difference, that passion alone won’t keep your doors open. Don’t forget the famous adage: no margin, no mission.”
Pink Floyd also equates money to a “hit”—and that could mean a hit in the sense of either a drug fix or a crowd-pleaser. That observation—while poetic—isn’t unique to classic rock-and-rollers. We all know the power, influence, and necessity of money. All too often, though, we shy away from it, allowing problems to fester and detrimentally impact our practices. Don’t turn such a blind eye that you end up having to shut your doors. Instead, follow the money. Monitor the above financial metrics to ensure the viability and profitability of your business.
Related posts

Why Experience and Expertise Matter for Rehab Therapy Software

Finding the Right ICD-10 Code For Sciatica

How to Use the ICD-10 Code for Difficulty in Walking

Learn how WebPT’s PXM platform can catapult your practice to new heights.

- Urgent Care Software Suite
- Urgent Care Connect
- Urgent Care Resources
- Experity EMR/PM
- DocuTAP EMR/PM
- Clockwise Patient Engagement
- Calibrater Patient Engagement
- DocuTAP Insight
- Experity Connected

Performance Metrics for Urgent Care
A successful urgent care venture requires understanding how well a center is performing over time, relative to budgets, and relative to industry benchmarks. Thus, urgent care entrepreneurs and operators need greater transparency than is provided by the monthly profit and loss statement. They need a consolidated view of financial and operational metrics that helps them pinpoint process, systems and staffing deficiencies requiring management intervention. Therefore, it’s no surprise that a frequent inquiry to the Urgent Care Association of America (UCAOA) is “which metrics are most important to track for an urgent care center?”
Business consultants have long advocated creating “scorecards” or “dashboards” that help managers determine whether an organization’s performance is meeting the expectations of owners, employees, customers, and other stakeholders. The following sections describe key financial and non—financial metrics that provide urgent care operators with a multi—faceted view of their center’s performance.
Get the 2021 eBook 10 KPIs to Watch in Your Urgent Care >>
Start with the Income Statement
Understanding the performance of any business starts with understanding the financial statements. Whether produced internally using desktop bookkeeping software or externally by a professional accountant, every urgent care operator should receive a standard financial package—Income Statement, Balance Sheet, and Statement of Cash Flows—on at least a monthly basis. Identifying meaningful management metrics begins by understanding these reports—particularly the Income Statement, which includes:
In reflecting upon the Income Statement, a cliché in business is that management should remain focused on the “bottom line” (meaning, “Net Income”). But Net Income is skewed by factors like how the business is financed and the corporate tax structure that do not reflect the performance of day-to-day operations. Expenses that are not directly related to the urgent care center’s “purpose” of treating patients are called “non-operating expenses.” An urgent care operator needs to understand how revenue coming in exceeds the amount of expenses paid to generate that revenue—and by taking out non-operating expenses; such is reflected in “Operating Income.”
Operating income is the most important line on the Income Statement because it’s a direct reflection of how well management influences revenue and controls expenses. Longitudinally, operating income is expressed as a percentage of Net Revenue—this ratio called “Operating Margin.”
EBIDTA goes a step beyond Operating Income to report the cash flow produced by operations. “Non-cash” adjustments like amortization and depreciation reduce Net Income but do not expend cash. Say, for instance, a center spends $10,000 for a new piece of equipment that is expected to last five years. Net income will be reduced by $2,000 per year—although the entire cash outlay occurred when the purchase was made. By taking out such “non-cash” adjustments to Net Income—EBIDTA reflects the true economic production of operations. As a result, EBIDTA is the primary measure used in valuing urgent care centers for sale. In performance reporting, EBIDTA is frequently expressed as a percentage of Net Revenue—called “EBIDTA Margin.”
Augment Financial Reporting with Operations Metrics
Financial reports like the Income Statement are based on transaction data passing through the accounting system so they represent the historic “summation” of a center’s performance. In order for a manager to know specifically where to focus his or her attention, financial data needs to be further expressed in the context of a center’s operations. The following metrics, calculated using the financial statement and operational data, illustrate the drivers of Operating Income:
Additional Details of Calculating Operations Metrics
When reporting patient visits and revenue, there is a risk that activity changes of component business lines (i.e. urgent care, occupational medicine, immigration physicals) or specific products (i.e. sports physicals, flu shots) will mask trends in the overall business and skew month-over-month and year-over-year comparisons. Consider the following examples:
- The center runs a promotion on high school sports physicals for $25. An influx of patients raises the visit count (denominator). But because the $25 generated by a sports physical (numerator) is less than the $150 realized from an urgent care visit—the report would show a decline in net revenue per visi This result obscure issues in coding, payer reimbursement, or billing/collections processes.
- Workers compensation and group health insurance visits are combined in patient revenue. The State implements a reduction in the workers compensation fee schedule resulting in a decrease of net revenue per patien Simultaneously, the center experiences an increase in an important group health contract. Because revenue remains flat, management fails to realize the financial impact of the reduced workers comp reimbursement.
The solution to these issues is to break down visits and revenue by major service lines and products. These may be reported as a “visit mix” or “revenue mix” percentage of total visits or revenue. Although this adds complexity to management reporting, the value is added insight to the operator on the revenue contribution of various business drivers. By contrast, because most expenses accrue to the center’s overhead, it’s typically not possible to calculate expenses attributable to specific products. Detailed analysis on the cost of delivering individual services is an exercise that should be performed on a periodic basis but it’s more information than is practical for management reporting.
Unless a center is open 365 days per year, typically operating days (days the center was actually open for business) are used in “per day” calculations as opposed to calendar days. Use of actual operating days can become cumbersome if reporting for multiple locations that are open different days, but the value is an apples-to-apple comparison of daily activity.
When calculating personnel counts, consider breaking down the number of FTEs by major job function such as physicians and physician extenders, support staff including nurses, medical assistants and technicians, and non-clinical staff such as front office specialists and the center manager. If staff members are cross-trained between the front and back office, allocate them (=1 FTE) by the percentage of time spent in each function (i.e. 50% FTE Medical, 50% FTE Non-Medical).
Contract personnel are typically included in FTEs counts for their respective job functions. However, if reliance on contract labor is due to extreme volume fluctuations (i.e. a flu epidemic) or problems in recruiting and retention—some operators find it useful to report contract labor separately. Personnel efficiency ratios can likewise be calculated by job function to pinpoint scheduling and efficiency problems among providers, medical support staff, and in the front office.
Integrate Non-Financial Metrics
The metrics discussed thus far represent measurable, numerically quantifiable activities. But there are additional, more subjective measures that represent how a center is performing relative to factors important to patients and employees. Like financial and operational metrics, these should be reported and followed on a monthly basis. Examples include:
Billing and Collections Metrics
Unlike “cash and carry” retailers and other service businesses, urgent care centers that bill insurance do not receive cash for the entire cost of services right away. There is typically an in-house or outsourced billing and collections function that converts the center’s patient “revenue” to “cash” by “working” Accounts Receivable. Timely and complete billing and collections is a center’s lifeblood — after all, a center can’t meet its payroll obligations using “Accounts Receivable.” To provide much needed transparency to management, billing and collections metrics should be incorporated into the monthly reporting package:
Longitudinal Reporting: Trend Analysis
After identifying which metrics to include in the monthly reporting package, the urgent care operator gains management insights by evaluating changes in metrics over time, relative to budget, and relative to industry benchmarks. Appendix 1 provides a sample set- up of the urgent care operating statement that incorporates these three analytical methods.
Urgent care revenue is generally determined by patient volume and the rate of reimbursement per patient. Expenses may be dependent upon volume (called “variable expenses”) or they may be “fixed” (unchanging, regardless of volume). Both fixed and variable expenses are subject to inflation. Trend analysis evaluates metrics over time to illustrate changes in revenues and expenses components to give the urgent care operator an idea of whether the business is performing better or worse, as well as the reasons why.
For example, the metric Operating Income Growth—calculated by dividing the current period’s operating income by that of the prior period—shows whether the center is becoming more or less profitable over time. Understanding changes in the component parts of operating income—a manager can clearly assess, for instance, that the center is more profitable due to increased reimbursement under an important payer contract, or alternatively less profitable due to the rising cost of employee benefits.
Variance to Budget
The simplest explanation of a budget is that it’s an “educated guess,” based on past performance, of how an urgent care center will perform in the future. Because budgets are used to allocate resources and hold managers accountable for generating revenue and controlling costs—it’s important each reporting period to evaluate a center’s performance relative to its budget. Because things happen during the course of operations that management could never anticipate, rarely will actual and budgeted numbers align perfectly. But seeing the discrepancies can lead the urgent care operator to ask probing questions, such as:
- Sales and marketing efforts
- Repeat visits due to patient loyalty
- Competition
- Flu epidemic
- Have there been any changes in payer mix or contracted rates among our major payers?
- Are we seeing any significant changes in patient acuity, ratio of new vs. established, or provider coding patterns?
- What trends are we seeing in employee turnover, staffing efficiencies, control of overtime and use of contract labor?
- Is there any unnecessary or excessive utilization we can curb in the center operation?
- Can we competitively bid or shop our vendor products to attain greater cost savings?
Metrics rarely provide the answers directly but they have tremendous value insofar as helping management identify the “right questions” to ask and then pointing them to potential solutions.
Ratio Analysis
Ratio analysis entails understanding the relationship between two or more items in the financial statements. For example, to understand how well an operator is managing the various expense components of a center, each may be reported as a percentage of Net Revenue:
When expenses are expressed as ratios, a center’s performance can more easily be compared to that of other centers—providing external validation and a “sanity check” for the center’s management. UCAOA, the Medical Group Management Association (MGMA), the American Academy of Family Practice (AAFP), and other groups frequently publish benchmarks that can be used to gauge the management of an urgent care practice.
Running a successful urgent care operation requires access to timely, accurate, and actionable performance data. Understanding the metrics that represent operational performance—as well as the drivers of operational performance—enables the urgent care operator to create a monthly reporting package that effectively tracks performance over time, relative to budget, and relative to industry benchmarks.
Learn more about modern KPIs. Watch the 2021 webinar KPIs to Measure in Your Urgent Care. On-demand now.
Watch the Webinar
Searching for a Simpler EMR Solution?
Experity’s EMR is built for Urgent Care, offering robust capabilities while remaining easy to use. With best-in-class onboarding and training, switching to Experity’s EMR has never been easier.
Recommended Posts

6 Benefits of Teleradiology Overread Services

Change Healthcare (Optum) Outage FAQs

Doctor’s Urgent Care Boosts Revenue with New EMR

Transitioning From Paper To Electronic Medical Records


Sign Up for the Urgent Care Minute
Join over 20,000 healthcare professionals who receive our monthly newsletter.

- Success Stories
- Meet the Team
- News & Resources
Financial Tools
Making Sense of Your Home Health Agency’s Financial Reports: Worksheets to Analyze Your Gross Profit & Margin by Cost Per Visit and Payer or Program
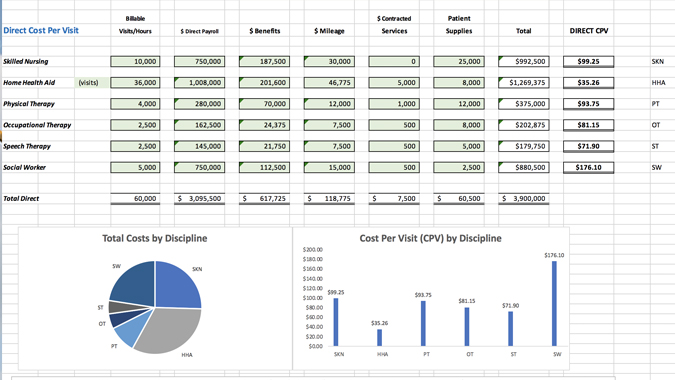
In my last post , we demonstrated how to calculate and evaluate gross profit in your agency. In this post, we look deeper at gross profit by type of service (or discipline) and do this analysis by payer of services.
Need a refresher? You can review my initial “how to calculate GPM” post here .
You may also view and download two handy worksheets below. But first, let’s review some basics.
Benefits of doing a GPM-by-CPV and GPM-by-Payer Analysis
The gross profit-by-service-and-payer analysis can be used to review a specific program within your agency. It can be modified to review a Hospice, non-medical home care or another program. You can also do this analysis by branch office or geographic area. You would simply use the applicable revenues and visits for the program, branch or geographic area you want to analyze.
It’s important to first understand your gross margin one or two levels deep – e.g. by type of service or discipline and by the payer of the services.
Look at specific payer information prior to renewing or renegotiating a contract. Know your profit dollars by detail. When negotiating, perhaps you don’t need an increase on physical-therapy but you must get one for home health aides. Or, perhaps you are not concerned with the therapy rates but really need an increase for your skilled nursing rates.
How much gross margin do you need? One answer is “As much as I can get”. But it’s essential to know the absolute requirements.
Look at Fixed & Semi-Variable Costs
Previously we discussed variable or direct costs, which increase or decrease relative to our business volume. Here we need to look at fixed costs – also labeled G&A, overhead, indirect costs, or whatever your accounting or finance department calls them. These include all costs that don’t change that much – either they are fixed (only increase once a year or more) or they are “semi-variable” and increase at certain steps in the growth (or decline) of the agency. Examples would include rent, telephone, office supplies, and management payroll. As examples, you would see increases (or decreases) in these expenses when you experience significant growth in census, or when you expand (or reduce) a certain program or decide not to accept a certain payer any longer.
A straightforward example: if you have $1,000,000 in gross profit and $900,000 in “fixed-type” expenses, then you have $100,000 of operating profit. Operating profit or operating income is the amount of profit (or loss) from operating activities. There may be other costs (or income) that are not directly related to operating activity that would be deducted or added to operating income to get to your net income (or loss). The net income (or loss) is your bottom line.
On the other hand, if you have $1,200,000 of fixed-type of expenses and $1,000,000 of gross profit dollars available to pay for them, you have an operating loss of $200,000.
The other way to look at this is to review your gross margin percentage. If your gross margin percentage is 30% of revenues and all of your fixed-type expenses add up to 32% of revenue, then you have a 2% operating loss.
Please focus on what you can do something about – control your gross profit! Be sure that you aren’t letting gross profit slip thru the cracks. It’s easy to let gross profit slide. The good news is that with the proper information, we can manage it.
Gross Profit MUST cover remaining expenses and leave something for profit!
Spreadsheets to get you started
Below is a two-tab spreadsheet (for cost per visit and payer) that can be used to calculate the direct cost per visit for each discipline. In completing this worksheet, we recommend that you use at least a three-month period of costs with matching revenues and visits. Try to get the best numbers you can on benefits and mileage by discipline. If necessary, use your best estimates. Most importantly, get your best estimate as to the cost for each type of visit your agency makes.
Once you have your cost per visit (CPV) you can start to evaluate your profitability by Payer. In the second spreadsheet, you can see an example of how this is calculated. By inserting the contracted net reimbursement rates for each payer, you can calculate the gross margin by discipline. You will likely find this very revealing. This is the perfect tool to use in your negotiations with payers. This will help you truly understand where you are making enough margin and where you are not covering the remainder of your costs.
Need support estimating your CPV and GM by Payer by Discipline? Reaching conclusions and/or taking action based on what your numbers reveal? Contact us at [email protected] or call 207-251-9661.
Click to download and plug your agency’s numbers into each schedule:
Cost Per Visit Analysis
Gross Margin by Payer by Discipline Analysis
Download PDF
Recent Financial Tools Articles
Your path to a successful plan starts here..
CONTACT US TODAY
Sign Up For Our Monthly Insights
Sign up for our e-newsletter and receive valuable insights for your care at home organization.
Schedule An In-Person Me eting
For those who are ready to meet face to face, and talk seriously about analyzing the financial operations of their agency.
SCHEDULE AN IN-PERSON MEETING
Schedule A Virtual M eeting
For those who aren't ready to meet face to face in-person but want to talk seriously about the financial operations of their agency.
SCHEDULE A VIRTUAL MEETING
14 Pond View Circle North Haven, CT 06473 203.691.1319 Contact Corcoran Consulting Group
Connect with us on LinkedIn Sign Up For Our Newsletter Connect with us on Google
Copyright © Corcoran Consulting Group, LLC. All Rights Reserved. Logos and imagery from other organizations for illustrative purposes only. Branding, digital and marketing by WORX . | Privacy Policy
- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes
You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
Understanding Copays, Coinsurance and Deductibles

Many or all of the products featured here are from our partners who compensate us. This influences which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .
Coinsurance, copays and deductibles are different out-of-pocket costs for health care, and being familiar with these terms can help you better understand your health coverage and costs. Even after you pay monthly premiums for health insurance , out-of-pocket costs can lead to high medical bills if you get sick or injured.
Here's how health insurance costs work.
Defining some health insurance terms
Before understanding how it all works together, let's brush up on some common health insurance terms.
Coinsurance
Coinsurance is a percentage of a medical charge you pay, with the rest paid by your health insurance plan, which typically applies after your deductible has been met. For example, if you have 20% coinsurance, you pay 20% of each medical bill, and your health insurance will cover 80%.
A copay, or copayment , is a predetermined rate you pay for health care services at the time of care. For example, you may have a $25 copay every time you see your primary care physician, a $10 copay for each monthly medication and a $250 copay for an emergency room visit.
The deductible is how much you pay before your health insurance starts to cover a larger portion of your bills. In general, if you have a $1,000 deductible, you must pay $1,000 for your care out of pocket before your insurer starts covering a higher portion of costs. The deductible resets yearly.
The premium is the monthly payment you make to have health insurance.
You pay the premium each month like a gym membership, even if you don't use the coverage. If you don't pay the premium, you may lose your insurance. If you're fortunate enough to have employer-provided insurance, the company typically picks up part of the premium.
Out-of-pocket maximum
The out-of-pocket maximum is the limit of what you'll pay in one year, out of pocket, for your covered health care before your insurance covers 100% of the bill. The maximum out-of-pocket limit for marketplace health plans (those on the Affordable Care Act health insurance marketplace) is $9,450 for an individual and $18,900 for a family in 2024 . (This amount doesn't include what you spend for services your insurance doesn't cover.)
Coinsurance vs. copay
Copays and coinsurance are different ways your health insurance may require you to pay for covered services. Here are the differences:
Copay vs. deductible
Your health plan may have both copays and deductibles, and whether you pay one or the other may depend on the services you receive. For some services, such as a visit to your primary care doctor, you may owe a fixed copay, such as $10 or $20. For other services, such as an MRI, you may have to pay the approved cost of the service up to your deductible.
Your copay may count toward your deductible, but it doesn't always. And you may owe copays for some services after you meet your deductible.
Coinsurance vs. deductible
Deductibles and coinsurance work together, but usually consecutively. As mentioned, the deductible is the amount you pay before your insurance starts covering the cost of your health care. Once you meet your deductible, you'll typically owe coinsurance (such as 20% of approved charges) on all additional services for the rest of the year.
You'll pay coinsurance on approved medical care until you hit the out-of-pocket maximum on your plan, after which your insurance will cover 100% of the rest of your care for the year.
How it all works together
Health insurance policies can have a variety of cost-sharing options. For example, some policies have low premiums, high deductibles and high maximum out-of-pocket limits, while others have high premiums, lower deductibles and lower max out-of-pocket limits.
In general, it works like this: You pay a monthly premium to have health insurance. Then, when you go to the doctor or the hospital, you pay either full cost for the services or copays as outlined in your policy. Once the total amount you pay for services, not including copays, adds up to your deductible amount in a year, your insurer starts paying a more significant chunk of your medical bills, commonly 80%. The remaining percentage that you pay is called coinsurance.
You'll continue to pay copays or coinsurance until you've reached the out-of-pocket maximum for your policy. At that time, your insurer will start paying 100% of your medical bills until the policy year ends or you switch insurance plans.
The catch: Your health plan's network
Here's the snag: The co-sharing scenario highlighted above works only if you choose doctors, clinics and hospitals within your health plan's provider network. If you use an out-of-network doctor, you could be on the hook for the whole bill, depending on which type of policy you have. This brings us to two related terms:
This is the group of doctors and providers who agree to accept your health insurance. Health insurers negotiate lower rates for care with the doctors, hospitals and clinics in their networks. So when you go in-network, your bills will typically be cheaper, and the costs will count toward your deductible and out-of-pocket maximum.
Out of network
A provider your insurance plan hasn't negotiated a discounted rate with is considered out of network. If you get care from an out-of-network provider, you may have to pay the entire bill yourself, or just a portion, as indicated in your insurance policy summary.
» MORE: What the No Surprises Act means for your medical bills
Doing the math on copays, coinsurance and deductibles
To illustrate with an example, consider a person — let's call her Prudence — who needs some health services. (Your costs would be different based on your policy, so you'll want to do your own calculations.)
Prudence's policy:
Insurance coverage: Single.
Annual deductible: $1,200.
Copays: $20 per office visit, $50 per specialist, $100 per ER visit; these don't count toward her deductible.
Coinsurance: 20% after she meets her deductible.
Scenario: Doctor visits and an MRI
Prudence goes in for an annual checkup. Because she goes to an in-network provider, this is a free preventive care visit. (If it had been an office visit for a medical issue, there would have been a $20 copay.) However, her primary care physician thinks Prudence should see an orthopedist based on her physical exam. The orthopedist later recommends an MRI.
Copays for an in-network specialist on her plan are $50. The MRI provider is in her insurer's network, and the approved insurance charge is $1,000 for the MRI, including the radiologist fees for interpreting the scan.
Imaging scans like this are "subject to deductible" under Prudence's policy, so she must pay for it herself, or out of pocket, because she hasn't met her deductible yet.
Total out-of-pocket costs: $50 for the specialist copay + $1,000 for the scan = $1,050.
Scenario: Trip to the ER
Later that year, Prudence falls while hiking and hurts her wrist. She heads to an in-network emergency room, for which she has a $100 copay. After the copay, ER charges are $3,400. Her deductible will be applied next.
Prudence has already paid $1,000 of her $1,200 deductible for her MRI, so she's responsible for $200 of the ER bill before her insurer pays a larger share. Of the remaining $3,200, her health plan will pay 80%, leaving Prudence with a 20% coinsurance of $640.
Total out-of-pocket costs: $100 for the ER copay + $200 for remaining deductible + 20% coinsurance ($640) = $940.
Prudence has now paid $1,990 toward her medical costs this year, not including premiums. She has also met her annual deductible, so if she needs care again, she'll pay only copays and 20% of her medical bills (coinsurance) until she reaches the out-of-pocket maximum on her plan.
Understanding how your health insurance works can save you money and grief now and down the road.
On a similar note...
Welcome To Our Blog
Industry insider insights from the professionals at uhc solutions..

How Much Revenue Do Primary Care Physicians Generate?
- HMG Success
- June 5, 2019

Any FQHC leadership team will tell you there is no mission without margin. Healthcare organizations of all types must pay close attention to the revenue-generating engines of their facilities. This includes physicians, who in addition to providing clinically effective care for patients, must also serve as the financial revenue generator for the facility.
But how much revenue can physicians generate, particularly for FQHCs?
Physician Revenue by Category
“FQHCs must evolve from their roots as “mission-first, margin-maybe” to organizations with a foundation of “no margin, no mission in order to be successful.” Sage Growth Partners
FQHCs typically employ doctors from the primary care specialties: Family Practice, Internal Medicine, Pediatrics, and General obstetrics/gynecology.
While the primary care doctors do not generate as much revenue as their surgical counterparts, Becker’s Hospital CFO Report tracks the revenue these providers generate for FQHCs, along with more invasive surgical specialists. The data comes from a 2016 Merritt-Hawkins report on physician salary surveys.
- Nationally, the average primary care doctor generates approximately $1.4 million in revenue for their organization annually. A specialist, on average, generates around $1.6 million each year.
- The highest producing physicians today are orthopedic surgeons. One full-time orthopedist can generate $2.7 million annually for their affiliated service provider.
- Coming in second is cardiology, whose clinicians generate the second-highest amount each year, at $2.4 million.
- Neurosurgeons followed cardiologists and general surgeons, generating $2.2 million on average for their facilities.
- However, primary care providers offer healthcare organizations great ROI. They fulfill a particularly important place in the healthcare safety net, serving as an important referral source to specialty providers. The primary care clinician is the entry point for most patients into the healthcare service delivery mechanism. Becker’s says these clinical providers may have a salary of around $198,000 annually; however, they generate 7.5 times the revenue, which is the highest of all clinical providers, including orthopedists.
Primary care providers generate extensive ROI via patient referrals, hospital admissions, tests and inpatient treatments. Healthcare providers note this as “downstream revenue,” which is particularly important to healthcare providers and their long-term fiscal solvency. This makes primary care providers both highly coveted and highly recruited by healthcare organizations. Dollar for dollar, the primary care provider is both a cost-effective clinician by salary output as well as a revenue generator for the healthcare system as a whole.
General Financial Impact of Doctors
The American Medical Association also quantified the general impact of all physicians on the communities they serve. They found that:
- Each year physicians generate $1.6 trillion for their healthcare system and the American economy.
- Each physician, no matter the specialty, supports on average 13.84 jobs.
- Doctors also support billions in annual wages, on average $1,076,462 per physician each year.
- The state and local tax income generated by physicians annually is $65.2 billion.
Above all, this data goes to show that physicians of all specialties are a value to the healthcare society and play an important role in the economy. UHC Solutions has hired many physicians over the years. Connect with our health center recruiting experts today about finding the right revenue generators for your team.
Search Blogs
Advance your career.
Find a unique opportunity just for you.
Start Your Talent Search
Trust us for your recruitment needs.
Get in Touch
We Look Forward To Connecting With You.
Diversity, Equity, and Inclusion
Learn about our commitment to DEI.

3 Centerpointe Drive, Suite 250 Lake Oswego, OR 97035
UHC Connector Sign-Up
Corporate members of:.

- Income Percentile Calculator for the United States
Below is an individual income percentile calculator for the United States in 2023. Enter pre-tax, gross income earned in full-year 2022 – January to December – to compare to the US individual income distribution. You can select to compare versus all workers, all workers who typically work 30 hours or more per week, or all workers who typically work 40 hours or more per week.
(For a complete picture, see the household income calculator ).
(Math and methodology in our average, median, and top 1% individual income post )
After try our income percentile by state and income percentile by city calculators. Or, switch to the household income calculator .
Individual Income Percentiles for the US Income Distribution in 2023
In this graph we developed for the average individual income post, we compare single-person earnings between 2022 and 2023.

(2022 numbers are CPI adjusted.)
What was the median individual income in 2023?
In the United States, median individual income was $50,000 in 2023.
What was the average individual income in 2023?
In the United States, average individual income was $69,029.61 in 2023.
What was the top 1% individual income in 2023?
The United States threshold for a top 1% individual earner was $407,500.00 in 2023.
In 2023, what was the threshold for the top 10% individual income in the United States?
The top 10% of individual earnings started at $135,605 in the United States in 2023.
In 2023, what was the threshold for the top 5% individual income in the United States?
The top 5% of individual earnings started at $187,506.00 in the United states in 2023.
How many people made $50,000 or more in 2023?
89,229,535 workers – 50.0% of the workforce – made $50,000 or more.
How many people made $100,000 or more in 2023?
33,510,143 workers, or 18.8% of all individual workers, made a six-figure income.
How many people made $250,000 or more in 2023?
4,946,579 workers, or 2.78% of the workforce, made a quarter million or more in income.
How many people made $500,000 or more in 2023?
.7% of workers, or around 1,328,910 people in the United States made a half million or more in income.
How many people made $1,000,000 or more in 2022?
Somewhere around 473,981 people made a seven figure income in 2023. That's less than .3% of the workforce.
(Talking about millionaires is usually more appropriate for net worth .)
What is considered a good individual income?
A good income in the United States started around $58,100 in 2023. That's the median individual income for a person who typically worked 40 or more hours per week . A high income is $95,004 , the 75th percentile of earnings for 40+ hour workers.
If you prefer to only look at salary – see the salary percentile calculator here.
These numbers are location dependent . In most of the country, they would provide you with a very good income. See our income by city post as income ranges vary widely by geography. (We also have income by state .)
Source and Methodology on the 2023 Individual Income Percentile Calculator
Sarah Flood, Miriam King, Renae Rodgers, Steven Ruggles, J. Robert Warren and Michael Westberry. Integrated Public Use Microdata Series, Current Population Survey: Version 10.0 [dataset]. Minneapolis, MN: IPUMS, 2022. https://doi.org/10.18128/D030.V10.0
For methodology, see the individual income bracket post. The only additional screens in this calculator were for workers reporting 30+ and 40+ hours a week or work, respectively – you can choose which one you like better for "full-time".
Want to see changes over time? Try our calculators from years past:
- 2022 US Individual Income Calculator
- 2021 US Ind i vidual Income Calculator
- 2020 US Ind i vidual Income Calculator
- 2019 US Individual Income Calculator
- 2018 US Individual Income Calculator
- 2017 US Individual Income Calculator
- 2016 US Individual Income Calculator
- 2015 US Individual Income Calculator
- 2014 US Individual Income Calculator
NEWSLETTER JOIN THE LIST
Popular in the last week.
- Minutes Calculator: See How Many Minutes are Between Two Times
- Hours Calculator: See How Many Hours are Between Two Times
- Week Calculator: How Many Weeks Between Dates?
- Month Calculator: Number of Months Between Dates
- Height Percentile Calculator for Men and Women in the United States
- S&P 500 Return Calculator, with Dividend Reinvestment
- Years Calculator: How Many Years Between Two Dates
- Age Difference Calculator: Compute the Age Gap
- Household Income Percentile Calculator for the United States
- Income Percentile by Age Calculator for the United States
- Least to Greatest Calculator: Sort in Ascending Order
- Net Worth by Age Calculator for the United States
- Average, Median, Top 1%, and all United States Household Income Percentiles
- Net Worth Percentile Calculator for the United States
- Income Percentile by State Calculator
- Stock Total Return and Dividend Reinvestment Calculator (US)
- Bond Yield to Maturity (YTM) Calculator
CLASSICS ON THE SITE
- Average, Median, Top 1%, and Income Percentile by City
- How Many Millionaires Are There in America?
- Stock Return Calculator, with Dividend Reinvestment
- Historical Home Prices: Monthly Median Value in the US
- Bond Pricing Calculator
Don't Quit Your Day Job...
PT Assistant Info
Search our nationwide database of resources for physical therapy assistants & students.
PT Assisting FAQ
Read FAQs on physical therapist assisting & ask the PTA community questions.
Local PTA Info
Find PTA salary data, license applications, board contacts & schools in your area.

A Student Career Guide to Becoming a Physical Therapy Assistant
How Much is a Physical Therapist Assistant Salary?
This page contains the most recent, complete, and accurate physical therapy assistant salary data provided by private employer surveys taken by the U.S. Bureau of Labor Statistics and presented by our team.
You can see how much a PTA salary is by city, major metro region, state, and also by the type of industry or healthcare setting.
✔️ Page updated: August 19th, 2023
Page Contents

If you are interested in a career as a PTA then use the salary data on this page to learn how much a physical therapy assistant salary is in your region and specific industry. The good news is that across the country PTA salaries are very competitive and often higher than many other similar healthcare careers’ salaries.
Average PTA Salary vs PT Salary
PTAs are paid very well compared to PTs who go through twice as much schooling . PT salaries are only about 33% higher than the PTA’s salaries who work for them, or about $16 more per hour.
PTA Salary by State
PTAs are earning a wide range of salaries in different states. Annual PTA salaries range from $49,240 to $78,920. Click a state to see the median PTA salaries in each state’s major cities.
PT Assistant Salary by City
The table below contains nearly 350 major cities and metropolitan areas with their corresponding physical therapist assistant salary data. Keep in mind that how much a physical therapist assistant makes will depend on many different factors aside from location such as industry and experience.
Top Paying Industries for PTAs
Physical Therapist Assistants are earning around $30 per hour in the top 5 paying industries they work in. Home healthcare services is currently the highest-paying sector for PTAs, as you can earn $78,360 per year which comes out to $37.67 per hour.
PTA Salary Outlook
Highest paying cities for physical therapist assistants.
You may want to know the cities offering the most income for PTAs so that you can make a career or move decision. Here are the 5 top paying cities in 2017 for a physical therapy assistant salary. Today in 2023, these are still some very well-paid areas to work.

- On average, PTAs in Lakeland earn a salary of $77,230 which is $25,070 higher than the average physical therapist assistant salary.

- In San Antonio, PTAs earn an average annual income of $75,840 which is $23,680 more than the median PTA salary.

- PTAs in Mcallen are earning $23,330 higher than the average PTA, which comes out to $75,490 per year.

- On average, PTAs in Modesto earn $20,150 higher than the average physical therapist assistant salary; bringing in $72,310 each year.

- PTAs in Victoria earn $19,540 more than the median salary for physical therapy assistants, coming out to $71,700.
Highest Paid Nonmetropolitan Regions for PTAs
If you prefer a non-metropolitan town, then working in Eastern or Northwestern Texas is the highest-paid location for you offering over $75,000 per year.
Physical Therapy Assistant Average Salary vs. Related Health Care Jobs
As you can see, those interested in a PTA career can expect to earn a highly competitive salary, especially for the cost of the shorter 2-year degree compared to a 4-year college degree. In fact, PTAs earn more than most other allied healthcare careers.
Here are some related healthcare salaries compared to a PTA average annual salary of $64,510 :
- Dental Assistants average $44,710.
- Medical Assistants bring in an average of $40,700
- Pharmacy Technicians’ average income is $40,260
- Nursing Aides earn an average salary of $36,220
Plus, becoming a physical therapy assistant always leaves you with the option of pursuing additional education to meet the requirements to become a physical therapist, who earns as much as $81,110 per year.
PTA Salary: Associate’s Degree vs Bachelor’s Degree
Some physical therapist assistants have an associate degree while others have a bachelor’s degree. Depending on the degree you hold and the PTA job that you have, you may earn a slightly different wage. Below is a PTA salary comparison for physical therapist assistants with associate’s degrees vs bachelor’s degrees with data provided from salary.com surveys to physical therapist assistants across the US.
- PTA Salary range with an Associate’s Degree: $55,787 – $59,770
- PTA Salary range with a Bachelor’s Degree: $58,064 – $61,066
All data presented here was collected by the Bureau of Labor Statistics, U.S. Department of Labor, Occupational Outlook Handbook, May 2022 Edition, Physical Therapist Assistants, on the Internet on this page
LATEST ARTICLES
Is Physical Therapy a Good Career?
By Steve Johnson
Physical Therapy Assistant Job Outlook & Employment Data
Top physical therapist personality traits and skills, pta info by state.
- PTA Schools
- PTA Salaries
- PTA Licenses
PT ASST. RESOURCES
- FAQ & Resources
- How to Become a PTA
- PTA Schooling
- What Does a PTA Do
- Should I Become a PTA
- Online PTA Programs
PTA Guide ™
Let Me Break Down How Much Ontario Doctors Really Get Paid

Family physician based on Madoc, Ont.
Have you ever wondered how much your family doctor is paid? Are not all doctors driving fancy cars, sipping fine wines and taking afternoons off to golf?
Most people are surprised to learn how little family doctors are paid for all of the services they provide.
How much do you think a family doctor is paid?
Would $32 per visit be fair? Would a flat rate of $16 per patient each month be fair?
Too much? Too little?
In 2015, Dr. Shawn Whatley wrote a pair of excellent blog posts that detail how much family doctors are paid. The following blog demonstrates two different examples of how family doctors are currently paid in Ontario.

Example 1: Fee for service billing
For decades, "fee for service" has been the traditional way that doctors bill OHIP for their services. Under this model, a doctor is paid a specific amount of money for a specific type of visit or procedure. For example, for a "minor assessment" such as a simple rash or skin spot, the physician would submit a bill to OHIP with the code A001 attached to it. They would then be paid the corresponding $21.70 in return. If a doctor stitches up someone's cut arm, she submits a bill for a code Z176 to OHIP, which pays the doctor $20.00 in addition to the assessment payment. A full list of services and payments can be found in this document from the Ministry of Health and Long Term Care.
There have been some further reductions since Dr. Whatley's blogs in 2015, though, and the payment figures in the link above aren't the most current numbers. The Ontario government unilaterally imposed cuts to physicians' payments a few years back — so, for instance, instead of being paid $33.70 for a typical visit (code A007 for an "intermediate assessment"), a family doctor is now paid $32.64.
Let us explore this further. Imagine a patient visits her family doctor for belly pain (for which the family physician would bill the most common code, A007, as noted above). Here are all the steps that are involved in such an assessment:
- Patient calls the doctor's office to book an appointment. (Remember: telephone lines and reception staff cost time and money, all paid by the doctor.)
- Patient visits the office, checks in with reception staff, is taken to exam room and prepared for the visit. (Again, staff are all paid by the doctor. Clinic rent, electricity, medical tools, equipment, etc. are all paid for by the doctor.)
- The doctor assesses the patient. (Remember: the doctor went to school for 10 or more years of education and training after high school in order to earn the expertise to care for her patients, not to mention the years of experience she has gained since.)
- The doctor orders blood work and an ultrasound in order to help diagnose the cause the of patient's belly pain. (To do this, the doctor needs to complete the appropriate paperwork to order the tests. All of this takes time, computer costs, faxing and/or telephone costs and more staff time.)
- The doctor may need to write a prescription for medications for the patient. (This takes time and expense of either paper or fax for the prescription.)
- The doctor needs to write a detailed note in the patient's chart to document the visit. (This takes more time and computer costs.)
- When the test results come back for the blood work, the doctor's staff receives them and puts them in the patient's chart, and then the doctor reviews them. (This takes staff time and doctor time.)
- When the ultrasound result is received, the staff puts the report in the patient's chart and then the doctor reviews the results. (This takes staff and doctor time.)
- The doctor then either calls the patient with the results or has her staff call the patient with results. (Again, this all takes doctor time, staff time and telephone costs, all paid by the doctor.)
For all of this time, cost and expertise, the family doctor is paid a total of $32.62 (but not quite, as she still has to pay taxes on income earned. Once corporate tax (if applicable) and personal income taxes are applied, the doctor only takes home as little as 54 per cent of the remaining profit).
Furthermore, the family doctor can only bill OHIP for one issue per day. So, if the patient also asks about an unrelated rash, or blood pressure control, or any other issue in that same visit, the doctor can still only bill that same $32.62.

Example 2: Capitated billing
In recent years, most family doctors are now paid for their services via "capitated" payment models. In a family health organization (FHO) model, a family doctor is basically paid a flat rate for looking after a patient for a year. This flat rate includes a specific list of services as well as some additional bonuses and incentives.
The amount of the flat rate varies depending on the age and sex of the patient. In my experience, a doctor is paid about $80 per year to look after a 20-year-old male patient, whereas she is paid about $440 per year to look after an 80-year-old female. On average, for the entire population, this works out to about $200 per year ($16.67 per month) per patient. This is a flat rate payment regardless of whether a patient visits the doctor twice — versus 10, 20 or even more times per year.
Sounds like a bargain — not to mention unsustainably undervalued.
In return for this total flat rate payment of $200 per average patient per year, the family doctor agrees to provide a list of 130 services. The extensive list these services can be found here in "Appendix A" (page 37 of 54).
Every single one of these visits, procedures and services requires staff time, doctor time and overhead costs, including the costs to buy all of the medical supplies and equipment. (Just as one example, it is worth noting that the supplies, nursing time and staff time required to perform a skin biopsy amounts to a total cost of $20 each).
In addition to the flat rate payment, the doctor may also earn an additional 15 per cent of the traditional fee for service payment. This is also known as "shadow billing." Using the most common example of a general assessment by a family doctor, the doctor would be paid a mere additional $4.90 (15 per cent of $32.64) for the visit.
More blogs from HuffPost Canada: Canadian Doctors Like Me Are Starting To Look For The Exit I Love Being A Doctor, But Canada Doesn't Love Me Hoskins Won't Survive The Mess He's Made Of Ontario Health Care
Given all of the above, and considering all of the education, training, skill, experience, responsibility, time overhead costs and taxes required to provide care for a patient, do you feel a family doctor deserves to be paid:
How's $32.64 per visit?
Perhaps just $16.67 per month?
From now on, when you hear of a physician billing $300,000 (or more) per year, just imagine how many patients are being treated and how much care is being provided. Imagine the hours, the responsibility and the overhead costs that are required to provide such service.
And imagine just how busy and hard-working that doctor must be.
Follow HuffPost Canada Blogs on Facebook
Also on HuffPost:
Support HuffPost
Our 2024 coverage needs you, your loyalty means the world to us.
At HuffPost, we believe that everyone needs high-quality journalism, but we understand that not everyone can afford to pay for expensive news subscriptions. That is why we are committed to providing deeply reported, carefully fact-checked news that is freely accessible to everyone.
Whether you come to HuffPost for updates on the 2024 presidential race, hard-hitting investigations into critical issues facing our country today, or trending stories that make you laugh, we appreciate you. The truth is, news costs money to produce, and we are proud that we have never put our stories behind an expensive paywall.
Would you join us to help keep our stories free for all? Your contribution of as little as $2 will go a long way.
Can't afford to donate? Support HuffPost by creating a free account and log in while you read.
As Americans head to the polls in 2024, the very future of our country is at stake. At HuffPost, we believe that a free press is critical to creating well-informed voters. That's why our journalism is free for everyone, even though other newsrooms retreat behind expensive paywalls.
Our journalists will continue to cover the twists and turns during this historic presidential election. With your help, we'll bring you hard-hitting investigations, well-researched analysis and timely takes you can't find elsewhere. Reporting in this current political climate is a responsibility we do not take lightly, and we thank you for your support.
Contribute as little as $2 to keep our news free for all.
Dear HuffPost Reader
Thank you for your past contribution to HuffPost. We are sincerely grateful for readers like you who help us ensure that we can keep our journalism free for everyone.
The stakes are high this year, and our 2024 coverage could use continued support. Would you consider becoming a regular HuffPost contributor?
The stakes are high this year, and our 2024 coverage could use continued support. If circumstances have changed since you last contributed, we hope you’ll consider contributing to HuffPost once more.
Already contributed? Log in to hide these messages.
Popular in the Community
From our partner, more in business.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Explore sell to government
- Ways you can sell to government
- How to access contract opportunities
- Conduct market research
- Register your business
- Certify as a small business
- Become a schedule holder
- Market your business
- Research active solicitations
- Respond to a solicitation
- What to expect during the award process
- Comply with contractual requirements
- Handle contract modifications
- Monitor past performance evaluations
- Explore real estate
- 3D-4D building information modeling
- Art in architecture | Fine arts
- Computer-aided design standards
- Commissioning
- Design excellence
- Engineering
- Project management information system
- Spatial data management
- Facilities operations
- Smart buildings
- Tenant services
- Utility services
- Water quality management
- Explore historic buildings
- Heritage tourism
- Historic preservation policy, tools and resources
- Historic building stewardship
- Videos, pictures, posters and more
- NEPA implementation
- Courthouse program
- Land ports of entry
- Prospectus library
- Regional buildings
- Renting property
- Visiting public buildings
- Real property disposal
- Reimbursable services (RWA)
- Rental policy and procedures
- Site selection and relocation
- For businesses seeking opportunities
- For federal customers
- For workers in federal buildings
- Explore policy and regulations
- Acquisition management policy
- Aviation management policy
- Information technology policy
- Real property management policy
- Relocation management policy
- Travel management policy
- Vehicle management policy
- Federal acquisition regulations
- Federal management regulations
- Federal travel regulations
- GSA acquisition manual
- Managing the federal rulemaking process
- Explore small business
- Explore business models
- Research the federal market
- Forecast of contracting opportunities
- Events and contacts
- Explore travel
Per diem rates
- Transportation (airfare rates, POV rates, etc.)
- State tax exemption
- Travel charge card
- Conferences and meetings
- E-gov travel service (ETS)
- Travel category schedule
- Federal travel regulation
- Travel policy
- Explore technology
- Cloud computing services
- Cybersecurity products and services
- Data center services
- Hardware products and services
- Professional IT services
- Software products and services
- Telecommunications and network services
- Work with small businesses
- Governmentwide acquisition contracts
- MAS information technology
- Software purchase agreements
- Cybersecurity
- Digital strategy
- Emerging citizen technology
- Federal identity, credentials, and access management
- Mobile government
- Technology modernization fund
- Explore about us
- Annual reports
- Mission and strategic goals
- Role in presidential transitions
- Get an internship
- Launch your career
- Elevate your professional career
- Discover special hiring paths
- Events and training
- Agency blog
- Congressional testimony
- GSA does that podcast
- News releases
- Leadership directory
- Staff directory
- Office of the administrator
- Federal Acquisition Service
- Public Buildings Service
- Staff offices
- Board of Contract Appeals
- Office of Inspector General
- Region 1 | New England
- Region 2 | Northeast and Caribbean
- Region 3 | Mid-Atlantic
- Region 4 | Southeast Sunbelt
- Region 5 | Great Lakes
- Region 6 | Heartland
- Region 7 | Greater Southwest
- Region 8 | Rocky Mountain
- Region 9 | Pacific Rim
- Region 10 | Northwest/Arctic
- Region 11 | National Capital Region
- Per Diem Lookup
FY 2024 Per Diem Rates Now Available
Please note! The FY 2024 rates are NOT the default rates until October 1, 2023.
You must follow these instructions to view the FY 2024 rates. Select FY 2024 from the drop-down box above the “Search By City, State, or ZIP Code” or “Search by State" map. Otherwise, the search box only returns current FY 2023 rates.
Rates are set by fiscal year, effective Oct. 1 each year. Find current rates in the continental United States, or CONUS rates, by searching below with city and state or ZIP code, or by clicking on the map, or use the new per diem tool to calculate trip allowances .
Search by city, state, or ZIP code
Required fields are marked with an asterisk ( * ).
Search by state
Have travel policy questions? Use our ' Have a Question? ' site
Have a question about per diem and your taxes? Please contact the Internal Revenue Service at 800-829-1040 or visit www.irs.gov. GSA cannot answer tax-related questions or provide tax advice.
Need a state tax exemption form?
Per OMB Circular A-123, federal travelers "...must provide a tax exemption certificate to lodging vendors, when applicable, to exclude state and local taxes from their hotel bills." GSA's SmartPay team maintains the most current state tax information , including any applicable forms.
PER DIEM LOOK-UP
1 choose a location.
Error, The Per Diem API is not responding. Please try again later.
No results could be found for the location you've entered.
Rates for Alaska, Hawaii, U.S. Territories and Possessions are set by the Department of Defense .
Rates for foreign countries are set by the State Department .
2 Choose a date
Rates are available between 10/1/2021 and 09/30/2024.
The End Date of your trip can not occur before the Start Date.
Traveler reimbursement is based on the location of the work activities and not the accommodations, unless lodging is not available at the work activity, then the agency may authorize the rate where lodging is obtained.
Unless otherwise specified, the per diem locality is defined as "all locations within, or entirely surrounded by, the corporate limits of the key city, including independent entities located within those boundaries."
Per diem localities with county definitions shall include "all locations within, or entirely surrounded by, the corporate limits of the key city as well as the boundaries of the listed counties, including independent entities located within the boundaries of the key city and the listed counties (unless otherwise listed separately)."
When a military installation or Government - related facility(whether or not specifically named) is located partially within more than one city or county boundary, the applicable per diem rate for the entire installation or facility is the higher of the rates which apply to the cities and / or counties, even though part(s) of such activities may be located outside the defined per diem locality.

IMAGES
VIDEO
COMMENTS
According to a study cited in this article from Advance Healthcare Network, the median annual income per square foot reported by participating physical therapy clinic owners was $203, with values ranging "from a low of $61 to a high of $550.". 5. Revenue per therapist.
A breakdown of the financials of a primary care clinic with income and expenses for the clinic for the past 6 months present. ... The government has assigned an RVU to each code. For example, a complex new outpatient visit is 3.17 work RVU's or 2.38 RVU's. There is a difference between (work RVU abbreviated wRVU) and (RVU). ... The average ...
Home Health Physical Therapy Per Visit Pay. Let's look at example of a week in the life of a home health PT who earns the following per visit rate: $90 per evaluation $80 per discharge $70 per follow up visit *Example: In an average day, let's assume you will see 6 patients. We'll say you have 1 eval, 1 discharge, and 4 follow up visits.
Revenue Per Visitor is a way to accurately assess average revenue per visitor to your website. The calculation is made by dividing the total income by the number of visitors during a specific time period. For example, if your income for January to March is $20,000, during which time you attracted 5,000 visitors, then your RPV would be $4.
The amount that it made on March 18th was $174, which I think is more accurate for the first day that it broke 10,000 visitors if that makes sense, so about $170, $174 in Ezoic earnings. That is an earnings per 1000 visitors of one day was $15.91 cents, the other day was $16.92 cents. I can jot those down. I'm going to get the average earnings ...
Overview. The Revenue per Visitor metric lets you track the total amount of revenue generated per single visit to your online store. Regularly monitoring the "Revenue per Visitor" e-commerce metric helps businesses understand the value of each visitor, measure the success of marketing efforts, and make data-driven decisions to optimize the user ...
Revenue per Visit is a performance metric that measures the amount of revenue generated by a website during a specific time period, divided by the number of visits to the site over that same period. ... Revenue is the total amount of income generated by the sale of products or services, as tracked by Google Analytics. It measures the monetary ...
Revenue per visitor is calculated by simply dividing the total revenue earned during a given time period by the number of visitors during the same time period. As a hypothetical example, if your revenue for the month of January is $10,000 and your site receives 2,000 visitors, your RPV would be $10,000/2,000 or $5 per visitor. Why RPV is important
Subtract all credits received from the total number of charges. (That way, you don't get an overly positive impression of your practice.) Divide the total charges, less credits received, by the total number of days in the selected period (e.g., 30 days, 90 days, 120 days, and so on). Divide the total receivables by the average daily charges.
Subtract the entire revenue from the total number of unique visitors to arrive at the RPV: Revenue per Visitor (RPV) can be computed using the following simple formula: RPV = Total revenue of website / Number of Unique Visitors. = $250,000 / 20,000 = $12.5. The RPV of $12.5 means that, on average, $12.5 was made by each person who visited the ...
Net income will be reduced by $2,000 per year—although the entire cash outlay occurred when the purchase was made. By taking out such "non-cash" adjustments to Net Income—EBIDTA reflects the true economic production of operations. ... Visits per Day and Revenue per Visit Operating Expenses per Visit: Personnel Counts: Total number of ...
Below is a two-tab spreadsheet (for cost per visit and payer) that can be used to calculate the direct cost per visit for each discipline. In completing this worksheet, we recommend that you use at least a three-month period of costs with matching revenues and visits. Try to get the best numbers you can on benefits and mileage by discipline.
The median per home-visit wage was $65.00 (n = 184) in home health agencies or clients' homes and $50.00 in outpatient clinics or offices (n = 51). The only function reported by a sufficient number of respondents was clinical service provider. Their median per home-visit wage was $62.00. (n = 232).
Salary with benefits: $45-48/hour (I was told during the phone screening I could negotiate to $52/hour, we'll see) Pay Per visit with benefits: SOC: $120 Recert/eval: $75 Treatment: $67. Both come with mileage reimbursement 65.5 cents/mile. Any insight would be extremely helpful as I have the official interview later this week! Archived post.
Federal income tax calculator. View all taxes. Tax credits and deductions; Tax forms; ... Copays: $20 per office visit, $50 per specialist, $100 per ER visit; these don't count toward her deductible.
After our auditing process, the average expected reimbursement per patient is $3,944.44. That means that Home Care Answers has helped our agency partners find an average of $320.61 per chart of additional, otherwise unclaimed revenue. This means that agencies are taking home more money and we can help quantify that gain.
Doctors also support billions in annual wages, on average $1,076,462 per physician each year. The state and local tax income generated by physicians annually is $65.2 billion. Above all, this data goes to show that physicians of all specialties are a value to the healthcare society and play an important role in the economy.
Below is an individual income percentile calculator for the United States in 2023. Enter pre-tax, gross income earned in full-year 2022 - January to December - to compare to the US individual income distribution. You can select to compare versus all workers, all workers who typically work 30 hours or more per week, or all workers who typically work 40 hours or more per week.
San Antonio, Texas - Average PTA Salary: $75,840. In San Antonio, PTAs earn an average annual income of $75,840 which is $23,680 more than the median PTA salary. McAllen, Texas - Average PTA Salary: $75,490. PTAs in Mcallen are earning $23,330 higher than the average PTA, which comes out to $75,490 per year.
In addition to the flat rate payment, the doctor may also earn an additional 15 per cent of the traditional fee for service payment. This is also known as "shadow billing." Using the most common example of a general assessment by a family doctor, the doctor would be paid a mere additional $4.90 (15 per cent of $32.64) for the visit.
There is a per diem rate for combined lodging and meal costs, and a per diem rate for meal costs alone. An employer may use either per diem method for reimbursing employee travel expenses. A self-employed person can only use per diem for the meal costs. Return to top 4. Do I include per diem payments in my employee's wages?
FICA contributions are shared between the employee and the employer. 6.2% of each of your paychecks is withheld for Social Security taxes and your employer contributes a further 6.2%. However, the 6.2% that you pay only applies to income up to the Social Security tax cap, which for 2023 is $160,200 ($168,600 for 2024).
Per diem rates. Rates are set by fiscal year, effective Oct. 1 each year. Find current rates in the continental United States, ... Please contact the Internal Revenue Service at 800-829-1040 or visit www.irs.gov. GSA cannot answer tax-related questions or provide tax advice. Need a state tax exemption form? Per OMB Circular A-123, federal ...