- Healthcare Services
- Find a Doctor
- Patient Portal
- Research and Education


Your recent searches
- Find a Location
- Nursing Careers
- Physical Therapy Careers
- Medical Education
- Research & Innovation
- Pay My Bill
- Billing & Insurance Questions
- For Healthcare Professionals
- News & Publications
- Classes & Events
- Philanthropy
How to Deal with Re-entry Anxiety and Post-pandemic Stress.
By Elspeth Cameron Ritchie, MD, Chair, Psychiatry
- Medstar Facebook opens a new window
- Medstar Twitter opens a new window
- Medstar Linkedin opens a new window
Find care now

If you are experiencing a medical emergency , please call 911 or seek care at an emergency room.
After more than a year of COVID-19 social restrictions, the U.S. pivoted from “you’re safer at home” to “get vaccinated and get back in action!” within a matter of weeks.
For some, the change was a major relief. But for many, the quick transition added fuel to a growing inferno of pandemic-related anxiety. Will I get sick if I return to the office? Is the vaccine safe? What if someone confronts me for wearing a mask?
Whether you are an introvert, extrovert, or somewhere in the middle, feeling a little rational anxiety —fact-based concerns—about “returning to normal” is expected and reasonable. However, excessive rational or irrational anxiety —unfounded worry—can prevent people from smoothly resuming social and career encounters that benchmark a healthy, happy life.
When I see patients for behavioral health care , I ask how the pandemic has affected them. Answers vary based on personal factors, such as whether they:
- Caught the virus or witnessed a loved one get sick
- Are suffering from long-term COVID-19 side effects, such as depression, memory loss, or “brain fog”
- Worked from home or in person with the public
- Lost their job
- Had their children at home 24/7
- Homeschooled their kids
- Took care of aging parents
- Were safe at home during lockdown
Even people who weren’t overtly affected personally by COVID-19 may be “languishing”—struggling to feel “normal” again after months of societal turmoil. The truth is, life is unlikely to revert to the “normal” we were used to, and that’s not necessarily a bad thing.
Despite the tragedies of the pandemic, some positive changes will hopefully continue, such as more choices for remote employment; increased telehealth options; and the precedence for staying home from work when we’re ill.
Still, rational and irrational anxiety is causing roadblocks for many people who want and need to move on from the pandemic. The good news is that re-entry anxiety is manageable when you are ready to start healing. Let’s discuss the differences between rational and irrational anxiety and what support services are available.
Post-pandemic #anxiety is a real and common problem. But help is available to manage the rational and irrational stressors of re-entering society. Elspeth C. Ritchie, MD, MPH, discusses tips to reclaim your quality of life: https://bit.ly/2UlFyQ9.
Click to Tweet
Rational vs. irrational anxiety.
Rational anxiety is rooted in truth. For example, at the time of this writing, the U.S. is widely lifting domestic travel restrictions. Simultaneously, new virus variants are emerging and we’re hearing news of catastrophic viral spread in Brazil and India. It’s natural to worry whether our country is on the right track.
Other rational pandemic-related fears may include:
- Going in public after having COVID-19: If you or a loved one were affected by the virus, it’s rational that you might be more concerned about spreading the virus or catching it again.
- Traveling by mass transit: Close proximity with others in an enclosed space can be a recipe for illness—a fact-based concern, regardless of the pandemic.
Irrational anxiety is characterized by unsubstantiated worry or fear when there is clear evidence to the contrary. In daily life, this may include hesitance to enter a tall building or feeling terrified by an innocuous sight or sound.
Irrational pandemic-related anxiety may include conspiracy theories, such as:
- Obsessive worry that Americans are being microchipped through the vaccine: More than 80% of U.S. adults use smartphones , which already enable geolocation. The idea of going to such great lengths for tracking is as unreasonable as it is unlikely.
- Fear of developing COVID-19 from the vaccine: This is scientifically impossible, since there is no actual virus, alive or dead, in any of the approved vaccines.
Both rational and irrational anxiety can absorb one’s thoughts, making it tough to focus, perform daily tasks, or even leave home. However, both can be treated with a thoughtful approach to how we perceive and react to pandemic-related stressors.
Related reading: How to spot depression and anxiety in teens.
8 anxiety management strategies.
Some patients with newly diagnosed or existing-but-worsened anxiety may benefit from medication. However, symptoms often can improve significantly with supportive, guided behavioral changes to help you regain control of anxious feelings.
1. Control the controllables.
A proven technique for managing anxiety is to focus on what you can control and minimizing what you can’t. Throughout the pandemic, many patients had trouble sleeping due to racing thoughts, such as an overwhelming fear that we were all going to die. I’ll admit, this worry crossed my mind at the beginning of the pandemic.
Yes, all of us will die someday. That is not something we can control. But what we can control is how we handle the present. I typically recommend that patients work through an internal dialogue about what they can and can’t control. This can help you find positives on which to focus your thoughts.
For me, my “controllable” was getting up, getting ready for work, and presenting my best self for my patients. What might “controllables” look like in your situation?
2. Practice deep breathing.
Take deep breaths through your nose and exhale out of your mouth. Repeat this 10 times. Focusing on manual breathing subconsciously refocuses your mind away from whatever was bothering you, if even for a moment. Deep breathing is a form of mindfulness, which is key to more sophisticated awareness practices, such as meditation.
3. Set healthy boundaries.
Several friends invited me to dinner a few weeks back. We’d all been vaccinated, but I requested that we all sit outside where it’s well-ventilated. I still preferred to wear my mask, and I decided in advance that I would leave early to avoid excessive hugging, handshakes, and crowds. What I told all my friends was that I had to be home at a certain time, and no one gave me a hard time about leaving before they did.
It’s up to you what you are comfortable with. Conversely, we owe it to each other to be kind if someone isn’t as ready as you to unmask or hang out at an event or in a restaurant.
Related reading: 6 signs you should be concerned about your mental health.
4. Exercise outdoors.
Moving and getting a change of scenery can help reset the mind and body. I enjoy walking around the koi ponds and flowers at MedStar Washington Hospital Center when I have a few moments between appointments.
If you live in Southern Maryland, you may have easy access to enjoy outdoor activities such as fishing, crabbing, canoeing, and boating. In Baltimore, you might catch a baseball game. Find an activity you enjoy and take your mind off worrying for a while.
5. Give back.
It can be tough to make yourself participate when you have anxiety. However, volunteering can temporarily replace racing thoughts by helping you focus on something positive. Animal lover? Volunteer at a pet shelter. Enjoy reading? Offer to read to kids at your local library. Worried about the homeless? Help out at a food bank. There’s always work to be done, and plenty of opportunities to help in your passion area.
6. Laugh a little!
At the start of the pandemic, I began carrying a stuffed lemur in the pocket of my hospital coat. Patients and colleagues would walk by, give me an odd look, then burst out laughing. Every time, I would beam ear-to-ear behind my mask. Laughing feels good, and it feels even better to make others laugh!
7. Prepare for naysayers.
There will always be a few people who feel it is their right to ridicule others for wearing or not wearing a mask as restrictions are lifted. At work, ideally you could turn to your boss or human resources professional to proactively manage or mitigate these situations. However, that’s not always possible.
If you feel comfortable speaking your mind, remain polite but firmly state, “I respect your decision. Please respect mine.” Sometimes it helps to plan out what you will say or do in certain situations. Role playing with your therapist or a friend can help build your confidence.
8. Take your time.
Whether you are anxious about returning to work or taking your first post-pandemic vacation, incremental steps are key. In our practice, we often recommend “extinction” or “exposure therapy,” which incorporates visualization to manage stressors.
For example, if a patient is afraid of crossing bridges, they’ll start with visualizing themselves crossing the bridge. Once they’ve mastered that, we arrange for them to cross a bridge with a loved one. Over time, they can work up to crossing solo. Some patients never cross alone, and that may be sufficient for them. The point is to set realistic, personally achievable goals you can stick to and go from there.
As we all adjust to our post-pandemic society, remember: Everyone’s timeline will be a little different based on their mental health and their experiences over the past tumultuous year. If anxiety is interfering with your life, don’t hesitate to seek help. We’ve been here for you, and we will be here—no matter what curveballs the next year throws our way.
Struggling with post-pandemic anxiety? The mental health team at MedStar Health is here to help. click below.
Request an Appointment
Stay up to date and subscribe to our blog
Browse by category.
- Behavioral Health
- Dermatology
- Gastroenterology
- Healthy Eating
- Heart and Vascular
- Living Well
- Neurology and Neurosurgery
- Orthopedics
- Physical Therapy
- Plastic and Reconstructive Surgery
- Primary Care
- Sports Medicine
- Womens Health
Latest blogs
Post-COVID Travel Anxiety
How to cope.

Dr Sarah Jarvis is the Clinical Director of the Patient Platform, an active medical writer, broadcaster, and the resident doctor for BBC Radio 2.
I think it's fair to say that for pretty much everyone, it has been a very strange couple of years. As the new decade dawned in January 2020, there were vague murmurings of a new infectious disease affecting parts of China. Within 3 months, the UK was locked down due to COVID-19 and travel had effectively ceased, at least where leisure was concerned. Even business travel pretty much halted – in the second quarter of 2020, UK air travel dropped by 97%.
While foreign travel remained off the cards, summer 2020 saw the rise of the staycation – promptly followed by a rise in COVID-19 cases and a second lockdown. The small number of people who did venture overseas lived with a constant risk of having to change their plans at short notice as new restrictions were introduced in response to rising cases.
Even in 2021, air travel in and out of the UK had slumped by 71% compared to pre-pandemic levels. For those who did decide to holiday abroad, there were seemingly endless changes to COVID-19 testing requirements and huge variations in regulations between countries.
So as the world opens up in 2022, it's hardly surprising that so many of us feel anxious. The newspaper headlines of the last 2 years mean that most of us have heard about the travel woes experienced by holidaymakers, even if we weren't among them. In addition, after 2 or even 3 years of not making regular holiday trips, we're no longer as familiar with the routine of packing essentials, checking flights, and coordinating travel plans with loved ones.
Be prepared
One of the key causes of anxiety is feeling out of control. And one of the best ways to avoid being out of control is to be prepared. That will allow you to breathe easy and enjoy your trip, confident that there won't be any nasty surprises in terms of COVID-19 regulations.
While COVID-19-related regulations for people in, and entering, the UK have gone, taking time to find out about regulations in the country you're visiting is an important first step.
There is no longer any need to take any COVID-19 tests or fill in a passenger locator form if you're travelling into the UK. This applies to Brits returning from holiday, as well as to people from other countries visiting the UK. There is also no difference in testing requirements depending on whether you've been vaccinated against COVID-19. That undoubtedly reduces complications, as you won't need to find a registered test centre while you're away or book a test to take shortly after you get home.
However, it is still very important to check the UK Foreign, Commonwealth & Development Office (FCDO) travel advice well before you go. In particular, their country-specific pages provide the latest COVID-19 travel advice for the country you're visiting. The number of countries with pandemic-related travel restrictions is shrinking all the time, but by checking in advance you can know you won't be caught out.
It's worth remembering that if you have a connecting flight, you'll need to find out if there are any different recommendations and requirements for any transit countries.
In the UK, there is no longer any legal requirement to self-isolate or report your results if you test positive for COVID-19. Nonetheless, self-isolating if you catch COVID-19 is still strongly advised, because of the risk the infection still carries (particularly to clinically vulnerable people and those who aren't vaccinated).
Of course, free Lateral Flow Tests are no longer available in the UK. But they are now available to buy for as little as a couple of pounds in the UK. In other countries, it may be harder to track down a Lateral Flow or PCR test.
So you may want to consider buying a couple of tests to take with you. This will mean that if you do develop symptoms that might be due to COVID-19, you can test yourself – and often be reassured that your test is negative, so you don't need to worry. It's worth thinking in advance about what you should do if you do test positive. For instance, does the hotel you're staying at have rules, and can they provide support for you to self-isolate?
Step by step
One of the great joys of holidaying abroad is the chance to sample new foods, whether it's local delicacies or popular 'imported' dishes such as pizza or curries, made in the way they were first designed. Usually, this is a treat - but if you haven't eaten out much in the last couple of years, the prospect of braving a crowded restaurant several times a day can be daunting.
A few simple steps will help make you feel more confident:
- Practice eating out. 'Exposure therapy' is commonly used by healthcare professionals treating people with anxiety. Eating out a few times in venues you're familiar with, close to home, will help you ease yourself into some aspects of eating with strangers.
- Quiet times. Find out from your hotel or restaurants you're considering when they are at their busiest. For instance, in many parts of Europe, it's common for people not to go out to dinner until late in the evening. In the USA, by contrast, restaurants may be packed at 6pm and have quietened down by 8.30pm. Plan your mealtimes to avoid the busiest periods.
- Go al fresco. We learnt within months of the pandemic starting that the risk of catching COVID-19 is much smaller outdoors than inside. Make the most of the balmy weather and the tradition of dining al fresco to eat outside. You may need to approach your hotel or restaurant in advance and explain your concerns – they will often be happy to oblige by reserving a table outside.
- To mask or not to mask? Wearing face coverings is no longer mandatory in the UK (except in some healthcare settings). Wearing a standard cloth face-covering doesn't offer you, the wearer, much protection. However, it does protect those around you. In many foreign countries, it's still standard for people to wear face coverings indoors. If this would make you feel safer, check with hotels and restaurants what their policy is.
Peace of mind
While the likelihood of becoming seriously unwell if you catch COVID-19 is much lower if you've been vaccinated, it is still important to make sure any medical problems are covered by your insurance. If you have medical conditions which you haven't declared – or don't have specialist travel insurance that covers you for those conditions – you could find your insurance is invalid if you need urgent medical help.
So for peace of mind, it's essential to know that you have insurance that will allow you to access care in any eventuality. And if you have any medical conditions, the best way to do that is to get insurance from a provider who specialises in providing cover for people with conditions such as yours.
The bigger picture
Of course, travel anxiety has been around since long before the pandemic. It's more common in people who have other mental health conditions, such as anxiety disorders or depression . However, there are also many people who cope perfectly with stress-inducing situations in the rest of their lives, but who struggle with travel anxiety.
- Share this page on Facebook
- Share this page on Twitter
Sign up to receive regular updates
Get the latest news, advice, travel tips and destination inspiration straight to your inbox.
- skip to Cookie Notice
- skip to Main Navigation
- skip to Main Content
- skip to Footer
- Find a Doctor
- Find a Location
- Appointments & Referrals
- Patient Gateway
- Español
- Leadership Team
- Quality & Safety
- Equity & Inclusion
- Community Health
- Education & Training
- Centers & Departments
- Browse Treatments
- Browse Conditions A-Z
- View All Centers & Departments
- Clinical Trials
- Cancer Clinical Trials
- Cancer Center
- Digestive Healthcare Center
- Heart Center
- Mass General for Children
- Neuroscience
- Orthopaedic Surgery
- Information for Visitors
- Maps & Directions
- Parking & Shuttles
- Services & Amenities
- Accessibility
- Visiting Boston
- International Patients
- Medical Records
- Billing, Insurance & Financial Assistance
- Privacy & Security
- Patient Experience
- Explore Our Laboratories
- Industry Collaborations
- Research & Innovation News
- About the Research Institute
- Innovation Programs
- Education & Community Outreach
- Support Our Research
- Find a Researcher
- News & Events
- Ways to Give
- Patient Rights & Advocacy
- Website Terms of Use
- Apollo (Intranet)
Coronavirus (COVID-19)
- Like us on Facebook
- Follow us on Twitter
- See us on LinkedIn
- Print this page
News May | 7 | 2021
Post-Pandemic Anxiety: Feeling Stressed as Things Return to Normal
As COVID-19 vaccinations roll out across the U.S. and states begin lifting various restrictions, many have begun thinking and dreaming of life post-COVID. And while the thought of gathering with family and friends again, traveling and getting back to loved activities can feel joyful, many are surprised to also feel stressed and anxious about the “return to normal.”
Soo Jeong Youn, PhD, a clinical psychologist in the Department of Psychiatry at Massachusetts General Hospital and an assistant professor in psychiatry at Harvard Medical School, discusses a few scenarios that can be a source of stress, and what people can do to help make the transition back into post-COVID life a bit easier.
COVID-19: Stressful or Traumatic?
While the pandemic has been a global event that has had an unimaginable impact on everyone’s life, not everyone has had the same pandemic experience. In some cases, the pandemic has been a source of trauma.
“A traumatic event is defined as actual or threatened death or serious injury by the DSM-5 ( Diagnostic and Statistical Manual of Mental Disorders , 5 th edition),” says Dr. Youn. “Depending on what your role is, what your job is, and how the pandemic has impacted you and your loved ones, you may have been exposed to a traumatic event.”
“But the important thing is that, regardless, everyone has been exposed to incredible stressors over the past year. We know that we're going to be dealing with long-term mental health consequences . The acute phase may be over, but we're going to be working through the chronic consequences for a while. Experiencing mixed reactions as we transition back is to be expected.”
Dealing with the Emotional Ebbs and Flows of COVID
These mixed reactions can be both situational and cyclical.
“Some people may have occasional worries that are contained to certain aspects of their life, or may be time limited” Dr. Youn says. “The beginning stage of constructing a 'new normal' is a period of transition. As we're building that new normal, there might be some worries and anxiety, but they dissipate as we get used to it all.”
For example, says Dr. Youn, being in larger groups of people or returning to the office after more than a year of isolating can be hard, especially if vaccination status is unknown, but may get easier over time. In other instances, transitioning back may feel fine, but then you may experience stress later. This is especially true for parents who may enjoy a less restrictive summer with their kids, but begin to feel anxious about their child’s personal safety, whether they’ve fallen behind academically or if their social connections with their friends have suffered as they head back to school.
It is important that as people go through this transition, they pay attention to how they are feeling and get help if needed says Dr. Youn.
“If a person notices that after a month or so there is no change whatsoever in how they are feeling, and they are experiencing very heightened levels of anxiety that is impacting their day-to-day functioning, their mood or their family, then they may want to consider talking to a mental health professional, especially if it is affecting multiple areas in their life.”
Gathering Again: How to Do So Safely
- Start slow: If you know that in a month’s time you’ll begin socializing with larger groups of people, meet with one person now and slowly grow your circle. Follow all COVID safety protocols like distancing and wearing masks, but begin interacting with people at a pace that is right for you to help lessen anxiety
- Know and maintain boundaries: Friends and family may have different comfort levels with different activities than you may have. In these cases, it is important to know your boundaries and clearly communicate them. These boundaries may shift depending on the situation and relationship, but the hope is that you are with people who will understand and come to an agreement on safety
COVID-19: A Gift of Time
For some, COVID-19 was a gift of time where they thrived. A slow-paced, flexible lifestyle may have helped them focus on themselves or family or work on individual goals that they didn’t have time for beforehand.
Dr. Youn offers advice on how to continue thriving when the pace picks up again: “Understanding first what were the components that were really helpful in succeeding under the circumstances is going to be important so that we can then figure out how to maximize those factors in the day-to-day. Now the trick is to figure out how to recreate those structures during the transition and build them into a normal life.”
A source of stress for others is the feeling that they did not use the COVID downtime in a productive way. While this may feel like a failure for some, Dr. Youn is clear: surviving the last year is a triumph.
“We cannot minimize the emotional and physical toll that the pandemic had on us,” she says. “It is going to be immeasurable for a long time. So whatever we did to truly survive the last year cannot and should not be dismissed. We have done everything that we can and we're here and wanting to rebuild a new future, whatever that may look like. That is a huge triumph.”
Related Links
- Tips To Improve Mental Health With Nutrition
- COVID-19 Vaccine Approval and Distribution FAQ
Centers and Departments
- COVID-19 (Coronavirus)
- Mental Health
Related News and Articles
- Press Release
- May | 23 | 2024
Century-old Vaccine Protects Type 1 Diabetics from Infectious Diseases
BCG-treated individuals had a significantly lower rate of COVID-19 infection compared with the placebo group and a significantly lower rate of infectious diseases overall.
- Apr | 15 | 2024
Research Spotlight: How Often Were Adults With Down Syndrome Listed as Do-Not-Resuscitate During the COVID-19 Era?
Researchers found that a person with a diagnosis of Down syndrome and COVID-19 pneumonia had six times the odds of having a Do Not Resuscitate (DNR) status ordered at hospital admission.
- Oct | 23 | 2023
Research Spotlight: Learning More About the Distribution and Persistence of mRNA Vaccines in the Body
Aram J. Krauson, PhD, of the Department of Pathology at Mass General, is the first author and James Stone, MD, PhD, is the senior author of a new study in NPJ Vaccines, Duration of SARS-CoV-2 mRNA Vaccine Persistence and Factors Associated with Cardiac Involvement in Recently Vaccinated Patients.
- Oct | 5 | 2023
Clinical Trial Reveals Benefits of Inhaled Nitric Oxide for Patients with Respiratory Failure Due to COVID-19 Pneumonia
Treatment improved blood oxygen levels and lowered the risk of long-term sensory and motor neurologic symptoms.
- Sep | 27 | 2023
Study Reveals More Depression in Communities Where People Rarely Left Home During the COVID-19 Pandemic
Results indicate a link between reduced mobility during the pandemic and greater risk for depressive symptoms.
- Aug | 10 | 2023
Transplant Recipients Experience Limited Protection With Primary COVID-19 Vaccination Series, but Third Dose Boosts Response
For lung and heart transplant recipients, vaccine doses beyond the third dose are likely important for maintaining immunity.

Post-COVID Anxiety Is Real
Here are 5 proven ways to beat it, and to benefit from post-traumatic growth..
Posted September 30, 2022 | Reviewed by Gary Drevitch
- What Is Anxiety?
- Find a therapist to overcome anxiety
- It's normal to experience anxiety trauma after a life-altering dangerous event.
- The key is to retrain your nervous system to strengthen the parasympathetic tone, or the calming response, as opposed to fight-or-flight.

Have you noticed that you have been more hypervigilant since the pandemic? And perhaps a bit more anxious in public? After a life-altering and life-threatening event, this is normal. Any shocking situation that involves life and death can lead to trauma.
Here's why people developed it during the pandemic: In many ways, Covid-19 trained us to become hypervigilant to contact with other people or potential contamination.
Clinically speaking, hypervigilance is a trait of anxiety . So, in many ways, the pandemic may have taught some of us to be hypervigilant to stay safe. In military contexts, service members are trained to be hypervigilant for safety, to seek out signs of danger, and to avoid potential threats. When they leave the military, they often find that even if they don’t have trauma symptoms, their hypervigilance remains because it was part of their training. For example, many veterans who have long left the military still locate exits whenever they enter a building or always keenly observe their environments for signs of danger. We might, then, expect those who endured the stress of the pandemic to remain anxious and hypervigilant for quite some time.
What can we do about this? The key is to retrain your nervous system to have a greater parasympathetic tone: the calming response, as opposed to fight-or-flight. When you do so, you might see that, from any traumatic experience, there can be post-traumatic growth .
Breathing exercises are a quick, efficient, and effective way to calm down anxiety by triggering the parasympathetic (“rest and digest”) nervous system. We come out of our sympathetic (“fight-or-flight”) response and return to a calmer state, our perspective broadens, and we can see things from a more rational perspective.
When you inhale, your heart rate increases. When you exhale, it slows down. Taking just a few minutes to close your eyes and lengthen your exhales (making them twice as long as your inhales) will help you calm down in minutes.
Our research has shown that one breathing technique, SKY Breath Meditation , can improve anxiety and depression while increasing well-being to a greater extent than other well-being practices, such as mindfulness . In addition. it may be a good complement or adjunct practice to traditional treatments for trauma.
Meditation: A regular meditation practice has been shown to improve stress, anxiety, and depression, boosting emotion regulation , well-being, and even physical health. The psychological benefits associated with meditation make it well worth trying out. Gentle Yoga, Tai Chi, Yoga Nidra—any physical movement or relaxation that settles the mind and induces a meditative state activates the parasympathetic nervous system. Regular practice trains your body to calm down faster and be calmer at baseline.
Nature: Exposure to nature has also been shown to profoundly benefit mental health , boosting well-being while lowering stress and anxiety. Even a limited amount of exposure can have a major impact. If you can't go out on a hike, having a poster of a nature scene on your wall can make a difference, as can a nature screen saver or a plant on your desk. That's how profoundly exposure to the natural world can impact us.
Compassion: Many studies have shown that being of service, in any capacity, improves your mental and physical health while contributing to longevity. Whether you are visiting a lonely aunt or volunteering at your local pet shelter, when you help others, it helps you . The impact of small acts of kindness or community service can be tremendous, even helping with recovery from disease.
Self-Compassion: So many of us are self-critical and hard on ourselves. In the process, we harm our mental and physical health, increasing our anxiety. Self-compassion involves treating yourself as you would treat a colleague or friend who may not have lived up to expectations in a given situation. Rather than berating, judging, and thereby adding to your friend’s despair, you would listen with understanding and encourage your friend to remember that mistakes are normal, without fueling the fire. Better mental and physical health, improved relationships, and a greater parasympathetic tone show the result of self-compassion.
To find a therapist near you, visit the Psychology Today Therapy Directory .

Emma Seppälä, Ph.D. , is a Lecturer at the Yale School of Management and is the author of SOVEREIGN: Reclaim your Freedom, Energy & Power in a Time of Distraction, Uncertainty & Chaos.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Dealing with travel anxiety in a post-COVID world
Travel has many benefits for our wellbeing but can be an overwhelming prospect post-covid. here’s how to manage travel anxiety, so you can get back out there..
Tags: Health COVID19 Achieving in life Real Wellbeing factors
“Travel is a coping mechanism that a lot of people have been without for quite a few years, which is contributing to that burnt-out feeling. It’s a reset time for your brain, and people who travel regularly do see the benefits in their mental health.”—Georgia Maling, Mental Health Coach, MindStep.
- Travel has significant benefits for our wellbeing, giving us something to look forward to and a fresh perspective on life.
- If you’re feeling anxious or stressed about travel, realise this is normal and aim to control the things you can control.
- Following COVID-safe guidelines is a proactive way to alleviate some of the stress of travelling.
The gently crashing waves. The hustle and bustle of an exotic city. The treks through rice paddies, over mountains and past ancient ruins.
However you choose to do it and wherever you go, travel is an act of self-care—a chance to unwind, reset and re-centre. At least, it was before the pandemic snapped borders shut, keeping us stuck in our suburbs, states and country.
Now that travel is back on the cards, it seems many of us are reluctant to take the plunge. So what’s standing in our way? And why is it worth facing our fears to get back out there?

Where did all our wanderlust go?
After being unable to travel abroad for more than two years, you’d expect people to be very eager to get out and about. But it seems almost the opposite is true, with international tourism down to a mere trickle.
It makes sense when you think about it, though. After all, many of us have already suffered repeated disappointments caused by the lockdowns of 2020 and 2021, while others may be anxious about the chance of contracting COVID or getting stuck overseas.
“Unfortunately, I think COVID over the past couple of years has made us quite hypervigilant to things that aren’t certain,” says Georgia Maling, a coach for mental health program MindStep, delivered by Australian Unity’s health division Remedy Healthcare. “So many people have had plans disrupted, particularly if you were living in Victoria, with the various sudden lockdowns that we’ve had and the cancelling of plans over and over and over again.
“I think people are quite cautious about that and the disappointment that comes along with it, so they’re trying not to expose themselves to the potential for that happening again.”
But, she adds, if you never expose yourself to the risks associated with travel, you’ll never get to experience the benefits and rewards that come along with it.
The Real Wellbeing benefits of travel
There’s nothing wrong with a bit of routine, but after a while the endless cycle of “eat, work, sleep, repeat” can be very draining, leading to feelings of numbness, fatigue and even burnout.
A change of scenery can help shake off stale energy, and planning the trip can give you something to look forward to, Georgia says. In her opinion, “researching accommodation, fantasising about what you’re going to do, eat and see—that’s half the fun!”
The time away can do wonders for your Real Wellbeing too, with travel being shown to reduce stress, improve brain function, increase creativity and boost mental health.
“Travel is a coping mechanism that a lot of people have been without for quite a few years, which is contributing to that burnt-out feeling,” Georgia says. “It’s a reset time for your brain, and people who travel regularly do see the benefits in their mental health.”

Come home reinvigorated, with a fresh perspective
Another benefit of travel is that it broadens your world view, giving your perspective a much-needed shake-up.
“It is known that your empathy increases when you see and experience different cultures and different ways of living,” Georgia says. “Seeing that diversity, making international friends, studying languages, different types of food and music—this all helps build your world view and your world perspective.”
You’ll come back refreshed and energised and will likely see your life in a whole new light, because “travel also gives you a greater appreciation for your own surroundings”.
How to manage travel-related stress in the COVID era
It’s perfectly normal to feel nervous about travel post-COVID—whether it’s thinking you might get sick, or just because it’s been a long time since you’ve done it.
But focusing disproportionately on things we can’t control causes anxiety and actually isn’t going to do you any favours.
“Anxiety and stress come from predictions about what may or may not happen in the future—and if your brain is working so hard to prepare for everything that may happen, that just sounds exhausting,” Georgia says. “It also means your travel is not going to be as pleasant an experience as it could be, and all those benefits will be overshadowed by the stress.”
Her advice is to instead focus on what you can do to troubleshoot some of your top concerns. For example:
- If you’re worried about getting stuck overseas, have a chat with your workplace about your capabilities to work remotely or the potential for flexibility to extend your plans if that does happen.
- Make sure you have enough funds to cover extended accommodation and other daily costs.
- Read over the terms of your travel insurance so you know what you’re covered for.

Following COVID-safe guidelines is another proactive way to focus your energy and attention, according to Steve Hollow, Head of General Insurance at Australian Unity .
“In terms of domestic travel, simply follow the COVID-safe advice—get vaccinated and boosted, wear masks when travelling in crowded spaces, such as public transport and planes,” he says.
Meanwhile, for international travellers, Steve has these top tips:
- Make sure you have travel insurance that protects you if you contract COVID before you travel or while you’re travelling.
- Check the government’s Smart Traveller website to understand the requirements of the destinations you want to travel to and follow the advice on the site.
- Take all the precautions you can to avoid contracting COVID in the first place.
There’s such a thing as being overprepared
While it always helps to be prepared, Georgia points out that it is possible to overdo it.
“Some clients tell me that they’ll double- and triple-check that they have everything in their suitcase before flying,” she says. “I think we’d all agree that one to two checks are sensible and reasonable, but once you get up to that third and fourth check it’s probably just adding to your stress and making you doubt yourself more.”
Besides, no matter how hard you try, there’s no getting around the fact that, from time to time, even the best laid plans can and do go awry. But, Georgia really believes that the upsides of travel outweigh the potential risks.
“Overall, just do it,” she says. “Taking some time away from work, seeing new places, it does release the stress that you’ve been holding onto—and releasing that stress and tension relaxes your mind and helps you to heal.”
Disclaimer: Information provided in this article is not medical advice and you should consult with your healthcare practitioner. Australian Unity accepts no responsibility for the accuracy of any of the opinions, advice, representations or information contained in this publication. Readers should rely on their own advice and enquiries in making decisions affecting their own health, wellbeing or interest. Interviewee titles and employer are cited as at the time of interview and may have changed since publication.
Remedy Healthcare Group Pty Limited and Australian Unity Health Limited are wholly owned subsidiaries of Australian Unity Limited.
An Australian Unity health partner, Remedy Healthcare provides targeted, solution-oriented healthcare that is based on clinically proven techniques. For more than 10 years, Remedy Healthcare has worked with more than 100,000 Australians – helping them to manage their health through caring, coaching, empowerment and support.
Related Articles

Need to know: all about chiropractic
From back and neck pain to headaches and more, chiropractors treat our body’s “mechanical” problems. Here’s your need-to-know guide to chiropractic.

What is osteopathy?
An osteopath takes a whole-body approach to help you treat or prevent injuries, aches and pains. Here’s what you can expect from osteopathy.

Taking a close look at endoscopy and gut health
A gastrointestinal endoscopy, or endoscopy for short, is a common medical procedure undertaken by many Australian Unity Members. But what is it, when is it used, and how is it used to improve gut health?
Supporting your wellbeing
Health services, wellbeing experts.
clock This article was published more than 3 years ago
How long will it take to overcome our pandemic travel anxiety?

Thomas Plante is grounded — by choice.
“The pandemic made me realize that I really would prefer not to travel at all,” says Plante, a psychology professor at Santa Clara University in Santa Clara, Calif.
Why stay home? Travel, with all its testing, quarantining and mask requirements, is a hassle. It’s also risky. People like Plante are turning inward, which is not only simple but safe.
“The pandemic has allowed reflection and discernment about a lot of things,” he says. “Travel is just one of them.”
Others apparently feel the same way. While the travel industry is abuzz with talk of pent-up demand and a historic resurgence, some erstwhile travelers are opting to stay home, possibly for good.
Miami psychiatrist Arthur Bregman says he has seen an uptick in patients who are reluctant to leave home as a result of the pandemic. He has coined a term for this feeling: “cave syndrome.”
“It’s about loving isolation to the point that you become dysfunctional,” Bregman says. “While this phenomenon is not directly connected to covid-19, it’s been exacerbated by the anxiety of uncertainty and its effects on our lives over the past year.”
For some, the disinclination is temporary. Travelers such as Alix Strickland Frénoy, an American who lives in Paris, are taking virtual trips. Her latest excursion, via laptop, took her to a number of castles, from the Château de Pierrefonds in the Oise, in northern France, to Miramare Castle in Italy.
“My husband and I love traveling virtually during the lockdown,” says Frénoy, who runs an educational website . “We haven’t done any actual physical travel in more than a year.”
For some travelers, the change feels permanent. Since the pandemic started, I have spoken with many readers who say they don’t see how they can go anywhere again and feel safe.
They’re people like Roslyn Hopin. Before the pandemic, she made plans to fly to Kazakhstan in fall 2020. But, at 89, Hopin felt that the risks of travel were too great and asked for a refund from Turkish Airlines. The airline returned her money in less than a week.
Hopin, a retired saleswoman from Delray Beach, Fla., does not expect to try again this year. “I had hoped to have this adventure in 2021,” she says. “But it does not look like it will happen.”
Definitely not. The U.S. Embassy in Kazakhstan has warned potential travelers to reconsider planned visits to that country because of the coronavirus , noting that its borders remain closed to foreigners, with limited exceptions.
Hopin says that she wants to travel again but that she’s concerned that it may not be safe to go anywhere for a while. Staying home is the only safe choice for her, at least for now.
I may have a touch of cave syndrome, too. I spent six months locked down in Sedona, Ariz., during the last surge. And I quietly congratulated myself for keeping my three kids safe while the virus raged outside. I firmly said no to weekend trips to California and day trips to the Grand Canyon. But by the fourth week, the travel writer in me was screaming, “Let me out!”
We finally pulled up stakes this month, embarking on a long road trip to the East Coast, but only after I had received both my shots. Part of me wanted to stay in Sedona until the pandemic ended.
Bregman says that after the 1918-1919 flu pandemic, some Americans suffered from what we would now call post-traumatic stress disorder. Although he has not seen anything as severe as PTSD in the general population’s reaction to this pandemic, there is a considerable amount of anxiety among his patients. In fact, it remains high even as the public health outlook improves. It’s manifested in your vaccinated friends who still won’t go out, he says. “They’ve fallen in love with their cave.”
So, do you have cave syndrome, or are you just playing it safe? Health and safety are among the most important considerations for travelers at this stage of the pandemic. They have to be included in any assessment of the risks and rewards of a vacation this year.
“It’s important to determine which variables are most important to you and your travel companions,” says Daniel Durazo, a spokesman for Allianz Travel , a travel insurance company.
If you want to err on the side of caution, you may want to stay in your cave for a little while. If the public health threat abates and you’re still struggling with travel anxiety, Bregman says, a combination of medication and therapy can help. And nothing puts you at ease quite like a carefully prepared plan, particularly when it comes to an upcoming trip.
Fortunately, our reluctance to travel is likely to fade with the pandemic, according to experts.
“However much Zoom and other technologies have advanced, the sights and smells of new places bring an excitement and opportunity for learning from others that can’t be replaced,” says Martha Merritt , the University of Richmond’s dean of international education. “As global travel becomes possible once again, I think many of us will return to it.”
Many — but not all.
Read more from Travel :
Read past Navigator columns here
Your Life at Home
The Post’s best advice for living during the pandemic.
Health & Wellness: What to know before your vaccine appointment | Creative coping tips | What to do about Zoom fatigue
Newsletter: Sign up for Eat Voraciously — one quick, adaptable and creative recipe in your inbox every Monday through Thursday.
Parenting: Guidance for vaccinated parents and unvaccinated kids | Preparing kids for “the return” | Pandemic decision fatigue
Food: Dinner in Minutes | Use the library as a valuable (and free) resource for cookbooks, kitchen tools and more
Arts & Entertainment: Ten TV shows with jaw-dropping twists | Give this folk rock duo 27 minutes. They’ll give you a musically heartbreaking world.
Home & Garden: Setting up a home workout space | How to help plants thrive in spring | Solutions for stains and scratches
Travel: Vaccines and summer travel — what families need to know | Take an overnight trip with your two-wheeled vehicle


Popular Services
- Patient & Visitor Guide
Committed to improving health and wellness in our Ohio communities.
Health equity, healthy community, classes and events, the world is changing. medicine is changing. we're leading the way., featured initiatives, helpful resources.
- Refer a Patient
5 tips to ease pre-travel anxiety
Author: Cheryl Carmin, PhD
- Health and Wellness
- Mental and Behavioral Health
- Neurological Institute

- Try to figure out what it is about travel that is making you anxious. What are you saying to yourself? Can you identify your “What ifs?” Once you’re able to understand what you’re afraid of, ask yourself if the fear is realistic. Even if your worst-case scenario is something catastrophic, does the very small likelihood of its occurrence outweigh the severity?
- If you have traveled before, what has your experience been? Did any of the things you’re worrying about happen? If they did, how did you manage? There’s a good chance you’re not giving yourself credit for being an effective and resilient problem solver.
- Is the over-planning, list-making or other strategies really helping? Everyone has their own way of preparing for travel. Making others conform to your way may cause arguments with your traveling companions and more stress.
- Do you have strategies to help you to relax? Slow, paced breathing is one strategy that many people find to be effective. Try an app for your smart phone, or one of the free relaxation recordings available from Ohio State’s Center for Integrative Medicine that help you to restore your calm equilibrium.
- Don’t skip the self-care activities. Just because you may think you’re in a time crunch the week before a trip, build in time for exercise. Physical activity is a great way to manage stress. Pamper yourself. A haircut or a manicure may be an important part of your pre-travel preparation to help you de-stress.
What provokes anxiety differs from person to person. This is definitely not a ‘one size fits all’ phenomenon. It may be useful to separate out if you’re afraid of the act of traveling or the destination.
- Our mental health experts are here to help you. Learn more
More from Ohio State

Anxious about returning to the post-pandemic world? You’re not alone
Mask or no mask? Is a hug OK? For some who have been diligent in avoiding social gatherings and crowds for so long, this return to a normal lifestyle is filled with anxiety.

Cicadas bugging you? You’re not alone. Read these tips to dial down your anxiety
Just the thought of billions of cicadas tunneling their way up to the surface is enough to seriously creep out people – some to the point where they won’t go in their backyard or to a park.

Facing Memorial Day grief, and why this year may be harder
This Memorial Day, some may be feeling the weight of loss more deeply. Memorial Day is about setting aside time to remember those we’ve lost. Giving ourselves space to feel the emotions that accompany those memories is important.
Visit Ohio State Health & Discovery for more stories on health, wellness, innovation, research and science news from the experts at Ohio State.
Check out health.osu.edu
Subscribe. Get just the right amount of health and wellness in your inbox.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Post-pandemic and post-traumatic tourism behavior
a Department of Integrated Resort and Tourism Management, Faculty of Business Administration, University of Macau, China
Jinyoung Im
b School of Hospitality and Tourism Management, Spears School of Business, Oklahoma State University, United States
Kevin Kam Fung So
Associated data, introduction.
The COVID-19 pandemic, a multi-faceted crisis and a potentially traumatic event, is both a personally impactful event and a globally shared experience (e.g., Williamson et al., 2021 ). However, exposure to highly stressful events can also be a precursor to post-traumatic growth, the positive personal growth people experience when emerging from adversity ( Tedeschi & Calhoun, 2004 ). In this perspective article, we aim to examine post-pandemic tourism behavior through the theoretical lens of post-traumatic growth. Casting COVID-19 as a catalyst for personal growth, we explore how post-pandemic travel and tourism activities manifest as the consequences of post-traumatic growth as well as the means for it. More importantly, we attempt to understand how post-traumatic growth and post-pandemic restructured assumptions about travel and tourism jointly influence the post-pandemic and post-traumatic tourism behavior.
Prior literature recognizes five major domains of post-traumatic growth: changed priorities and a deeper appreciation of life; development of closer social relationships; resilience; openness to new life possibilities; and greater existential or spiritual growth ( Tedeschi & Calhoun, 2004 ). Post-traumatic growth entails a process of shattering the old “assumptive world,”—one's general understanding of the world—and restructuring the fundamental components of a new one in its place. The COVID-19 pandemic has been a seismic force of disruption to the act of travel. Restrictions in movements, border closures, cancellations of flights and other transportation means, and closures of tourist destinations have drastically shattered the pre-pandemic assumptions people held for travel and tourism. The pandemic also accelerated some geopolitical trends such as de-globalization, isolationism, and regionalism. In this research, we present a set of seemingly opposing behavioral tendencies in an attempt to capture the imprints of post-traumatic growth and restructured assumptions about travel on post-pandemic tourism behaviors. Namely, rebound and retreat, connectedness and estrangement, and self-transcendence and self-diminishment in post-pandemic and post-traumatic tourism behavior.
Rebound and retreat
Post-traumatic growth reflects coping with the lingering distress of the trauma and attempts at psychological survival ( Tedeschi & Calhoun, 2004 ). In the post-pandemic era, travel and tourism patterns are likely to mirror post-traumatic growth's initial stage of return to baseline, recovery, and reset. As the pandemic abates and travel restrictions start to ease, a sudden surge in travel and tourism activities in the initial post-COVID period is expected. For example, on June 11, 2021, more than two million people screened through U.S. airport security checkpoints in a single day, which more than doubled the number in April 2020 and was close to 75% of the volume recorded on the same day in 2019 ( Koenig, 2021 June ). The predicted sudden and dramatic rebound in travel demand is vividly described as “revenge travel” in the media ( Bologna, 2021 April ). Such burning urge to travel also has psychological roots, signifying travelers' need for retribution against COVID-19 and a regained sense of control to return to normalcy.
As tourism rebounds, retreat behavior in tourism is also likely to be salient. With a heightened sense of vulnerability induced by the pandemic, retreat behavior of the “6 foot-tourism world,” or the disconnection between tourism spaces and reframing tourism activities on a local scale ( Lapointe, 2020, p. 636 ), manifests in behaviors such as maintaining social distancing from other travelers, avoiding overly popular tourism destinations, choosing less-known tourism destinations, and preferring regional travels. Solitary travel experiences such as camping in remote areas ( Bhalla et al., 2021 ) and travel centered on retreat experience ( Wang et al., 2021 ) are likely to continue to gain popularity after the pandemic. Solo travels that are unconstrained by interpersonal decision making and motivated by solitary experience are on the rise as well ( Shin et al., 2022 ).
Connectedness and estrangement
One of the most noticeable domains of post-traumatic growth is developing closer relationships with others ( Tedeschi & Calhoun, 2004 ). The relationship domain of post-traumatic growth will be particularly salient in the post-COVID era. The COVID-related movement restriction measures, such as suspension of social gatherings and travel bans, have resulted in a sense of social disconnectedness ( Kato et al., 2020 ). Visiting immediate family and friends is likely to be a strong travel motivation that drives the first wave of travel in the immediate wake of the pandemic. Increasing demand in multi-generational travel may also be expected.
While the tourism industry will benefit from post-traumatic growth in building stronger interpersonal relationships, of particular significance is the simultaneous social estrangement induced by the pandemic at interpersonal, community, national, and international levels. At the interpersonal level, moments of subtle hostility and belligerence are found in various leisure situations. For example, a visitor without a mask assaulted a native elderly person in Hawaii ( Bourlin, 2021 March ). At the destination level, residents' “us versus them” mentality has been reignited. Many countries have banned cruise ship arrivals at their ports ( Fox, 2021 February ). At the national and international levels, deglobalization, isolationism, and the regionalism of tourism ( Brouder et al., 2020 ) will have opposing effects on tourism development. Tourists may also display xenophobia that leads to reduced international travel, hesitation to try foreign food, and greater preference for using a travel agency and group travel ( Kock et al., 2019 ). The localized and regionalized travel trends due to nationalistic thoughts, distrust, anxiety, and even hostility have intensified during the pandemic ( Brouder et al., 2020 ) and may have a long-term adverse effect on post-pandemic travel and tourism.
Self-transcendence and self-diminishment
Catastrophic events drastically alter people's outlooks in life as people make sense of events, search for meaning and purpose, and seek spiritual growth ( Tedeschi & Calhoun, 2004 ). Given its severity, the COVID-19 pandemic could be considered as existential hapax, a crucial moment of life and an intense experience that led to significant physical, emotional, and spiritual transformation ( Matteucci, 2021 ). In the post-pandemic era, travel for purpose and morality may become more prevalent as people engage in a deeper introspective reflection in searching for purpose and constructing a revised life narrative. The COVID-19 pandemic has exacerbated many social issues such as unequal access to health care, poverty, food insecurity, racial injustice, and more. A notable phenomenon during the pandemic is the occurrence of large-scale protests despite the risk of spreading the virus ( Berger, 2020 October ). New forms of activism-based tourism are emerging, such as justice tourism and protest tourism ( Guia, 2021 ). For example, in August 2020, Portland, Oregon in the United States saw an increase in the number of tourists who came to visit the sites of the Black Lives Matter protests ( Gallivan, 2020 August ). The focus of alternative tourism is social eudaimonia that highlights compassion, ethics, and collective well-being ( Matteucci et al., 2021 ).
The Covid-19 pandemic induces direct health threats as well as secondary stressful events stemming from pandemic-related circumstances such as financial distress, separation from one's social support system, and a prolonged pandemic without an end in sight ( Williamson et al., 2021 ). Such wide-spread stressors can lead to negative psychological responses such as depersonalization (a sense of detachment from self, others, and the world) and a sense of self worthlessness ( Williamson et al., 2021 ). Such self-diminishment tendencies may manifest in tourism behaviors such as lack of interest in travel and reduced enjoyment when they do.
This research offers a post-traumatic growth theoretical perspective of post-pandemic tourism behavior ( Fig. 1 ). While the post-pandemic and post-traumatic tourism behaviors are presented as outcomes of both pandemic induced and post-traumatic induced changes, it is important to recognize that the two forces are often intertwined. For example, pandemic-induced risk reduction (retreat) behaviors are conceptually related to post-traumatic growth. While current literature predominately approaches post-traumatic growth as a general measure (e.g., the post-traumatic growth inventory, Tedeschi & Calhoun, 1996 ; the traumatic life events questionnaire, Kubany, 2004 ), this research demonstrates that trauma-specific restructured assumptions might interact with the generic domains of post-traumatic growth to bear on domain-specific (i.e., travel and tourism) post-traumatic growth.

A conceptual framework of post-pandemic post-traumatic tourism behavior.
This research may offer implications for other crises that threaten tourism such as natural disasters, terrorism, and military conflicts. Miao et al. (2021) provided a terror management perspective of COVID-19 travel and tourism behavior. The post-traumatic growth perspective offered by this research extends the literature by portraying post-pandemic travel and tourism behavior as conscious efforts against mortality. Different degrees of such traumatic events experienced by individuals may manifest in different tourism behaviors. For example, people with a lower degree of risk perception toward COVID-19 intend to travel longer and more frequently ( Kim et al., 2021 ).
Future research can build on the theoretical foundations laid out by this study to test the relationships between post-pandemic tourism behavior and post-traumatic growth. Another fruitful inquiry is to what extent post-pandemic travels trigger feelings of traumatic growth and which forms of travel are most effective in inducing such effects. In addition, future researchers can take a qualitative approach through in-depth interviews and personal narratives to explore the connections between post-pandemic tourism activities and post-traumatic growth.
Declaration of competing interest
Biographies.
Li Miao is a professor at University of Macau, focusing on travel and tourism behavior.
Jinyoung Im is an assistant professor at Oklahoma State University, interested in consumer
Kevin Kam Fung So is an associate professor at Oklahoma State University, interested in
services marketing.
Yan Cao is a doctoral candidate at Oklahoma State University, interested in consumer behavior.
Associate editor: Jeroen Nawijn
Appendix A Supplementary data to this article can be found online at https://doi.org/10.1016/j.annals.2022.103410 .
Appendix A. Supplementary data
The following is the supplementary data related to this article.
Post-pandemic and post-traumatic tourism behavior.
- Berger M. The Washington Post; 2020, October 2. The pandemic is an ear of protests—And protest restrictions. https://www.washingtonpost.com/world/2020/10/02/coronavirus-pandemic-demonstrations-protest-restrictions/
- Bhalla R., Chowdhary N., Ranjan A. Spiritual tourism for psychotherapeutic healing post COVID-19. Journal of Travel & Tourism Marketing. 2021:1–13. [ Google Scholar ]
- Bologna C. Huffpost; 2021, April 6. ‘Revenge travel’ will be all the rage over the next few years. https://www.huffpost.com/entry/revenge-travel-future_l_6052b724c5b638881d29a416
- Bourlin N. Sfgate; 2021, March 27. ‘Your vacation is my home’: Hawaii's residents are speaking out against tourists behaving badly. https://www.sfgate.com/hawaii/article/hawaii-residents-locals-tourists-behaving-badly-16056414.php
- Brouder P., Teoh S., Salazar N., Mostafanezhad M., Pung J., Lapointe D., Desbiolles F., Haywood M., Hall C.M., Clausen H. Reflections and discussions: tourism matters in the new normal post COVID-19. Tourism Geographies. 2020; 22 (3):735–746. [ Google Scholar ]
- Fox A. Travel + Leisure; 2021, February 28. Canada extends ban on cruise ships until at least 2022. https://www.travelandleisure.com/cruises/canada-bans-cruise-ships-until-2022
- Gallivan J. Portland Tribune; 2020, August. Wish you were here: Portland sees surge in protest tourism. https://pamplinmedia.com/pt/9-news/475933-384307-wish-you-were-here-portland-sees-surge-in-protest-tourism
- Guia J. Conceptualizing justice tourism and the promise of posthumanism. Journal of Sustainable Tourism. 2021; 29 (2–3):502–519. [ Google Scholar ]
- Kato T.A., Sartorius N., Shinfuku N. Forced social isolation due to COVID-19 and consequent mental health problems: Lessons from hikikomori. Psychiatry and Clinical Neurosciences. 2020; 74 (9):506–507. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kim E.E.K., Seo K., Choi Y. Compensatory travel post COVID-19: Cognitive and emotional effects of risk perception. Journal of Travel Research. 2021:1–15. [ Google Scholar ]
- Kock F., Josiassen A., Assaf A.G. The xenophobic tourist. Annals of Tourism Research. 2019; 74 :155–166. [ Google Scholar ]
- Koenig D. AP News; 2021, June. Travel rebound: 2 million people go through US airports. https://apnews.com/article/coronavirus-pandemic-technology-health-lifestyle-travel-a2b3260a8633c2404dab44507b5de811
- Kubany E. Western Psychological Services; Los Angeles, CA: 2004. Traumatic life events questionnaire and PTSD screening and diagnostic scale. [ Google Scholar ]
- Lapointe D. Reconnecting tourism after COVID-19: The paradox of alterity in tourism areas. Tourism Geographies. 2020; 22 (3):633–638. [ Google Scholar ]
- Matteucci X. Tourism Recreation Research; 2021. Existential hapax as tourist embodied transformation; pp. 1–5. [ Google Scholar ]
- Matteucci X., Nawijn J., von Zumbusch J. A new materialist governance paradigm for tourism destinations. Journal of Sustainable Tourism. 2021:1–16. [ Google Scholar ]
- Miao L., Im J., Fu X., Kim H., Zhang Y.E. Proximal and distal post-COVID travel behavior. Annals of Tourism Research. 2021; 88 [ Google Scholar ]
- Shin H., Nicolau J.L., Kang J., Sharma A., Lee H. Travel decision determinants during and after COVID-19: The role of tourist trust, travel constraints, and attitudinal factors. Tourism Management. 2022; 88 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tedeschi R.G., Calhoun L.G. The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996; 9 (3):455–471. [ PubMed ] [ Google Scholar ]
- Tedeschi R.G., Calhoun L.G. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004; 15 (1):1–18. [ Google Scholar ]
- Wang Y.C., Chen P.J., Shi H., Shi W. Travel for mindfulness through Zen retreat experience: A case study at Donghua Zen Temple. Tourism Management. 2021; 83 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williamson R., Hoeboer C., Primasari I., Qing Y., Coimbra B., Hovnanyan A., Grace E., Olff M. Symptom networks of COVID-19 related versus other potentially traumatic events in global sample. Journal of Anxiety Disorders. 2021; 84 [ PMC free article ] [ PubMed ] [ Google Scholar ]
Post-Pandemic Anxiety: Life is Returning to Normal, So Why Do You Feel Anxious?
- Share to Facebook
- Share to Twitter
- Share to LinkedIn
- Share on Email

You’re fully vaccinated, New York is reopening, and life is getting back to normal. So, why are you anxious? Instead of joy, you feel overwhelmed, stressed, and can’t stop asking yourself: How should I behave around others? Should I continue to physically distance? Should I shake a stranger’s hand? Do I even want to?
After more than a year of social distancing and without knowing who is fully vaccinated, returning to ‘normal’ may feel scary, especially if you already live with anxiety, according to Dr. Susan Evans, Professor of Psychology in Clinical Psychiatry. “Anxious individuals worry,” Dr. Evans says. “Whenever there is uncertainty about the future, there is the likelihood for increased worry and anxiety,” she says.
Are you a productive or unproductive worrier?
Worry is a ruminative process that takes the form of ‘What if…,’ which is usually some negative and often catastrophic prediction about something bad happening, Dr. Evans explains. During the pandemic, much of people’s worry has been safety related and presented as questions such as, “’What if I get sick…?” “What if I wasn’t careful enough…?” “What if someone in my family gets infected?”
The pandemic and its imperative to socially distance have also triggered or intensified social anxiety, which breeds worry about how others perceive you and leads to questions like, “What if they don’t like me…?” “What if I say something stupid…?”
There has also been an upswing in overall anxiety about job safety, going out of business, loss of income, or even housing. “People are more worried than ever about their financial situation,” Dr. Evans says. Longstanding and newly aggravated societal, cultural, and political problems have multiplied this anxiety, she says. “Health and economic disparities, social injustice, and gun violence are all serious matters that people are worried about.”

The COVID-19 anxiety cycle
Despite growing optimism about the course of the COVID-19 pandemic, and the rollout of vaccines that are proving to protect against some variants, television news and social media focus on the negative: how vaccine resistance may undermine efforts to achieve ‘herd immunity;’ rising infections from COVID variants; and concerns about the longevity of vaccine-derived immunity. “For anxious individuals, the default position is to ruminate on worst case scenarios,” Dr. Evans says. “Rumination leads to more anxiety and so it becomes a vicious cycle.”
To interrupt the cycle, it helps to understand the difference between productive and unproductive worrying, Dr. Evans explains. “Unproductive worry is about focusing on things that might happen and spinning in your head about it. Productive worry is asking the question, “Is there anything I can do about this now?” and then taking the appropriate action.”
For example, ruminating and feeling anxious over whether you can handle returning to your office is unproductive worry, whereas deciding to take one day at a time and focus on the present moment is productive. “It is important to address the problem of avoiding life and engage in work and other activities that are considered reasonable and safe,” she says.
Similarly, worrying about your risk of catching COVID (very low if you’re fully vaccinated) now that states and localities are relaxing most pandemic-related capacity restrictions, and the U.S. Centers for Disease Control (CDC) has given fully vaccinated people the green light to go mask-less--except in certain crowded settings and venues--when enjoying other outdoor activities alone or with family members, is unproductive, whereas taking action to continue wearing a mask and socially distance is productive.
Taking small, positive steps
Knowing all of this may help lessen--but not erase--your anxiety and depression, which may linger for a while. In the meantime, Dr. Evans suggests easing back into life at your own comfort level.
“If you have been isolating and have not been outdoors, start with small steps such as walking to the corner,” she advises. “Practice building on this experience as your confidence grows. Keep in mind that having one foot out of your comfort zone is a good thing because it suggests you are stretching yourself.”
Practicing mindfulness is a useful skill to cope with general anxiety, she continues. “Mindfulness is about paying attention, on purpose, in the present moment. Paying attention to the present moment is the opposite of ruminating and being stuck in one’s head in unproductive worry.”
To cope with specific anxiety about returning to work, school or socializing, Dr. Evans suggests building your stress resistance by getting enough sleep, exercising, practicing yoga and or meditation, or talking to a friend.
She also warns against excessive intake of the media, particularly social media, as well as over-indulging in alcohol or food. “Anxious individuals may use substances to avoid the way they are feeling so be careful of excessive alcohol or other emotion numbing strategies such as overeating.”
As you work through your anxiety, try to remember that you are not alone. The pandemic has struck everyone in one way or another and many people may be feeling as anxious as you.
If you have previously struggled with anxiety or depression, then you may want to seek professional help. You may join a group therapy program to work on your social anxiety. Whatever you do, try to practice self-compassion and care, and don’t feel compelled to hide your feelings. Sharing them will encourage others to share theirs, which may help you to feel better and less alone in the long run.
Related Links
Back to News
In This Article
Clinical service.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 19 June 2024
Chronic post-COVID neuropsychiatric symptoms persisting beyond one year from infection: a case-control study and network analysis
- Steven Wai Ho Chau ORCID: orcid.org/0000-0002-2986-8677 1 , 2 ,
- Timothy Mitchell Chue 1 ,
- Rachel Ngan Yin Chan 1 , 2 ,
- Yee Lok Lai ORCID: orcid.org/0009-0004-1002-8805 1 ,
- Paul W. C. Wong 3 ,
- Shirley Xin Li 4 ,
- Yaping Liu ORCID: orcid.org/0000-0002-2015-8775 1 , 5 ,
- Joey Wing Yan Chan ORCID: orcid.org/0000-0002-2692-2666 1 , 2 ,
- Paul Kay-sheung Chan 6 ,
- Christopher K. C. Lai ORCID: orcid.org/0000-0001-8591-5944 6 ,
- Thomas W. H. Leung 7 &
- Yun Kwok Wing ORCID: orcid.org/0000-0002-5745-5474 1 , 2
Translational Psychiatry volume 14 , Article number: 261 ( 2024 ) Cite this article
360 Accesses
17 Altmetric
Metrics details
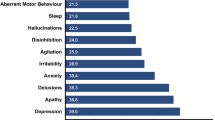
- Psychiatric disorders
Our study aims to delineate the phenotypes of chronic neuropsychiatric symptoms among adult subjects recovering from their first COVID that occurred more than one year ago. We also aim to explore the clinical and socioeconomic risk factors of having a high loading of chronic neuropsychiatric symptoms. We recruited a post-COVID group who suffered from their first pre-Omicron COVID more than a year ago, and a control group who had never had COVID. The subjects completed app-based questionnaires on demographic, socioeconomic and health status, a COVID symptoms checklist, mental and sleep health measures, and neurocognitive tests. The post-COVID group has a statistically significantly higher level of fatigue compared to the control group ( p < 0.001). Among the post-COVID group, the lack of any COVID vaccination before the first COVID and a higher level of material deprivation before the COVID pandemic predicts a higher load of chronic post-COVID neuropsychiatric symptoms. Partial correlation network analysis suggests that the chronic post-COVID neuropsychiatric symptoms can be clustered into two major (cognitive complaints -fatigue and anxiety-depression) and one minor (headache-dizziness) cluster. A higher level of material deprivation predicts a higher number of symptoms in both major clusters, but the lack of any COVID vaccination before the first COVID only predicts a higher number of symptoms in the cognitive complaints-fatigue cluster. Our result suggests heterogeneity among chronic post-COVID neuropsychiatric symptoms, which are associated with the complex interplay of biological and socioeconomic factors.
Similar content being viewed by others
Long COVID prevalence and impact on quality of life 2 years after acute COVID-19

Dimensional structure of one-year post-COVID-19 neuropsychiatric and somatic sequelae and association with role impairment
The effects of the COVID-19 pandemic on neuropsychiatric symptoms in dementia and carer mental health: an international multicentre study
Post-acute COVID syndrome (PACS), also known as ‘Long-COVID’, is a major global health concern [ 1 ]. While SARS-CoV-2 is primarily a respiratory virus, COVID is now recognised as a multisystem disease [ 2 , 3 ]. Neuropsychiatric symptoms are among the most common non-respiratory symptoms both in the acute phase of COVID and PACS, such as mood and anxiety symptoms, sleep disturbance, fatigue and cognitive complaints [ 4 ]. Available evidence suggests that the risk of increased incidence in several neuropsychiatric conditions occurs not only within the first few months of SARS-CoV-2 infection, but can also extend up to a year beyond infection [ 5 ]. Recent studies have also shown changes in the brain post-SARS-CoV-2 infection. A longitudinal MRI study, for example, has demonstrated structural brain changes after SARS-CoV-2 infection [ 6 ]. MRI imaging studies have suggested grey matter or cortical changes among those suffering from PACS [ 7 , 8 ]. The way SARS-CoV-2 infection affects brain health in the long term, however, is not well understood. Currently, the prevailing hypothesis links neuropsychiatric symptoms of PACS with neuroinflammation and prolonged immune dysregulation triggered by SARS-CoV-2 infection, and/or microvascular pathology secondary to endothelial dysfunction [ 9 ].
Significant knowledge gaps also exist regarding chronic neuropsychiatric sequelae after SARS-CoV-2 infection. First, most PACS studies have focused on the first year after SARS-CoV-2 infection, leaving questions about post-COVID symptoms that run a chronic course, which is arguably a major public health concern. Second, while many PACS studies have simply considered neuropsychiatric complaints as part of a unitary PACS syndrome, this approach may overlook the heterogeneity of diverse experiences under the PACS umbrella, as well as unique factors associated with different symptom groups. For example, while preliminary evidence suggests that clinical factors, such as infection severity and COVID vaccination, are predictive factors for PACS [ 10 ], socioeconomic factors and pre-existing mental illness are often neglected in the PACS literature. Third, there have been very few studies thus far that attempt to delineate the phenotypes of chronic neuropsychiatric aspects of PACS by exploring the relationship among subjective neuropsychiatric symptoms and corresponding quantitative mental and cognitive measures.
In response to these gaps in knowledge, our current study aims to use a symptom-based approach, supplemented by validated symptoms, health-related quality of life (HRQoL) measures and app-based cognitive tests, to delineate the phenotypes of chronic neuropsychiatric symptoms among young to middle-aged adult subjects recovering from their first, pre-Omicron strain SARS-CoV-2 infection that occurred more than one year ago. We also aim to explore the relationship and clustering among common chronic neuropsychiatric symptoms, and to test if these clusters are associated with different risk factors. We set out the following hypotheses: (1) Post-COVID subjects would have a higher level of neuropsychiatric symptoms, worse neurocognitive performance and worse HRQoL 1 year after being first infected by SARS-CoV-2 compared to control subjects who had never been infected by SARS-CoV-2; (2) Clinical factors such as the severity of the index infection, vaccination status, and socioeconomic status will be associated with the level of chronic neuropsychiatric complaints persisting beyond one year of the index infection among post-COVID subjects; (3) Chronic neuropsychiatric symptoms among post-COVID subjects will form clusters discoverable by network analysis.
Subjects for the post-COVID group and the control group were concurrently recruited in the community from 24 August 2022 to 1 March 2023 via posters in hospitals, online advertisements via social media, and university email newsletters. All advertising material was available in both Chinese (in traditional characters) and English language. The inclusion criteria for the post-COVID group were as follows: (i) report history of a laboratory-confirmed SARS-CoV-2 infection which occurred before January 2022 (i.e. before the Omicron variant became dominant in Hong Kong) [ 11 ]; (ii) first SARS-CoV-2 infection occurred at least one year prior to the study, and; (iii) age between 18–65 years. Inclusion criteria for the non-COVID control group were as follows: (i) no history of SARS-CoV-2 infection as confirmed by lateral-flow test or PCR; and (ii) matched with the post-COVID group in terms of the following 5 characteristics: age, gender, ethnicity, pre-OVID medical and psychiatric comorbidities, and socioeconomic status (primarily measured by the locally developed Deprivation Index, which measures material deprivation and has been widely used for local public health research [ 12 , 13 ]). All participants gave written informed consent either in person or via videoconference. We then instructed all participants to install a mobile phone app designed for this study. Using the app, participants completed (i) a set of questionnaires on their demographic information and socioeconomic and health status at two time points: December 2019, which was immediately before the COVID pandemic reached Hong Kong [ 11 ], and at the time of the assessment; (ii) a PACS symptoms checklist that comprised of 15 neuropsychiatric items and 26 non-neuropsychiatric items (see Supplementary materials for full checklist): the choice of items was based on results from earlier PACS studies [ 4 ], and we subsequently classified the severity of subjects’ acute COVID into three categories: (a) asymptomatic or mild, for subjects who did not have symptoms of pneumonia; (b) moderate, for subjects who had symptoms suggestive of pneumonia (i.e. presence of fever, cough, and shortness of breath) but did not require oxygen therapy; and (c) severe or critical, for subjects who had symptoms suggestive of pneumonia and required oxygen therapy and/or intensive care; (iii) a set of questionnaires on standardised mental health, sleep and HRQoL measures as follows: Patient Health Questionnaire-9 (PHQ-9), General Anxiety Disorder-7 (GAD-7), Impact of Event Scale-revised (IES-r) [ 14 ], Insomnia Severity Index (ISI) [ 15 ], Chalder Fatigue Scale (CFS) [ 16 ], CAGE screening questionnaire for alcoholism, Global Physical Activity Questionnaire (GPAQ) [ 17 ] and WHOQOL-BREF (excluding the environmental domain) [ 18 ]; (iv) a seven-day sleep diary; and (v) app-based cognitive tasks focusing on key domains (concentration, psychomotor speed and working memory) related to the phenomenon of ‘brain fog’ [ 19 ], which included the psychomotor vigilance test (PVT), digital symbols substitution test (DSST), N-back test, and alternate finger-tapping test (see Supplementary Method for test instructions and scoring methods). The application was available in Chinese(in traditional characters) or English depending on the subjects’ preference. Subjects who completed all assessments were compensated with HKD$150 (~USD$20) in supermarket coupons. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects were approved the Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee (Ref.: 2022.362). The study protocol was registered on the ISTCTN registry on 8 September 2022, which can be accessed at: https://doi.org/10.1186/ISRCTN35268189 .
Data analysis
We tested for univariate between-group differences in demographics, socioeconomic and health status, and symptom score between the post-COVID group and control group using t-test, chi-square test or their non-parametric equivalent. To differentiate between post-covid subjects with a high or low symptom load, we used weighted Wasserstein distance to define a cut-off point, such that the group with a symptom number below the cut-off point (the ‘low symptom load group’) had the closest level of mental health and sleep distress, HRQoL and cognitive task performance as compared to the matched control group. The high symptom load group was then defined as the group with a symptom number above the cut-off point. To calculate the Wasserstein distance, the weights for each measurement were taken from the regression coefficients of the logistic regression model that separated the post-COVID subjects from the control group. We then performed a univariate between-group differences analysis in demographics, socioeconomic and health status, and symptom score between the high and low symptom load groups using t-test, chi-square test or their non-parametric equivalent. We used a multivariable regression model to look for potential predictors after adjusting for potential confounders.
To explore the relationships among chronic post-COVID neuropsychiatric symptoms and their clustering patterns, we built a regularised partial correlation network based on the data from the post-COVID group in relation to self-reported neuropsychiatric symptoms [ 20 , 21 ]. To minimise the instability of the network, we excluded symptoms suffered by fewer than or equal to 20 people (out of a sample of 223 people). After network estimation, we used the walktrap algorithm to discover the communities/clusters within the symptom network. To validate the robustness of the detected communities, we used the community assortativity (r_com) metric, a bootstrapping procedure, to measure the robustness of community assignments done by the walktrap algorithm . Community assignments are deemed to be robust if r_com is larger than 0.5 [ 22 ]. We used R packages of bootnet , IsingFit, igraph, ggraph and plyr to perform the network estimation process, and asnipe and assortnet for assortativity metric estimation. For details about the network estimation and validation procedures, please see Supplementary Method .
We recruited 223 post-COVID cases and 224 non-COVID control subjects (see recruitment flowchart in Supplementary Material ). For the post-COVID group, the mean duration from index infection to assessment was 757 days (range = 371–1105 days). The majority of the post-COVID subjects had no known pre-COVID physical or mental comorbidities (80.7 and 95.5%, respectively) (see Supplementary material for the full list of symptoms and their frequency), and the majority of them (70%) suffered from no or mild respiratory symptoms during the acute phase of their first COVID infection. 25% of the subjects had suffered from at least one re-infection. There were no statistically significant differences in key demographics and pre-pandemic socioeconomic and health status between the post-COVID and control groups (Table 1 ).
The differences in the level of depressive, anxiety, post-traumatic stress and insomnia symptoms between the post-COVID and control groups did not reach statistical significance. The post-COVID group, however, had significantly more fatigue symptoms than the control group (bimodal scoring; median = 3.0 vs 2.0, U value = 29830.5, p < 0.001) despite a similar daily sleep duration. The HRQoL measures of the two groups were comparable. In relation to app-based cognitive tasks, there was no statistically significant difference between the two groups in terms of their performance in the PVT and N-back tasks. The post-COVID group performed worse in the DSST (median of total accurate count = 58.0 vs 60.5, U value = 21565.5, p = 0.013) and the alternate finger-tapping task as compared to the control group (median of total accurate count = 34.0 vs 41.0, U value = 21540.0, p = 0.012) (Table 2 ).
The post-COVID group had more newly diagnosed medical conditions since the beginning of the COVID pandemic (mean = 0.14 vs 0.05, U value = 26782.5, p = 0.0062), but not psychiatric diagnoses (see Supplementary material for the full list of symptoms and their frequency). They also had more days of hospitalisation in the past year (median = 0 vs 0, mean = 0.9 vs 0.2, U value = 26370.5, p = 0.048) but not more medical consultations. The post-COVID and control groups did not have statistically significant changes in socioeconomic status, as reflected by changes in the Deprivation Index and subjects’ employment status.
Among patients who were infected by the SARS-CoV-2 virus, 60% reported at least one neuropsychiatric symptom which appeared during the acute or early post-recovery period of their first COVID infection and has persisted until now. The most frequent complaints were memory problems (50.2%), fatigue (31.8%), inability to concentrate (30.5%), anxiety (21.1%), insomnia (20.6%), post-traumatic stress (PTS) (18.4%, as measured by IES-R), daytime sleepiness (17.5%) and feeling depressed (15.2%) (Table 3 ).
Defining symptom load groups
The levels of depression, anxiety, fatigue, insomnia, PTS, as well as HRQoL measures, but not cognitive performance, worsened as the number of chronic neuropsychiatric symptoms reported increased (see Supplementary material ). The weighted Wasserstein distance analysis showed that post-COVID subjects with less than four persistent neuropsychiatric complaints were closest to the matched control group in terms of the level of mental and sleep problems, HRQoL and cognitive task performance (Fig. 1 ). Thus, post-COVID subjects with less than four persistent symptoms were defined as the low symptom load group, while those with four symptoms or more were defined as the high symptom load group.

The weighted Wasserstein distance between the group with their number of symptoms below different cut-offs and the matched control group. The cut-off symptom number that results in the shortest distance is the optimal cut-off to define the high/low symptom load groups.
According to this cut-off, 67 of our subjects (30%) had a high symptom load (Table 2 ). There were no statistically significant differences in the baseline characteristics of the high and low symptom load groups, although the mean age of the high symptom load group was nominally higher (mean = 44.8 vs 41.1, U value = 5993.2, p = 0.083), and the difference in pre-COVID levels of social deprivation between the groups approached statistical significance (median = 1.0 vs 1.0, U value = 6008.5, p = 0.065). The median number of pre-morbid medical conditions and the presence of known psychiatric conditions in the two groups were similar, though the high symptom load group had a higher number of persistent non-neuropsychiatric symptoms after the acute phase of COVID infection (median = 6 vs 0, U value = 9577.5, p < 0.001) (Table 1 ).
The high symptom load group had a statistically significantly higher number of newly diagnosed medical conditions (median = 0 vs 0, mean = 0.3 vs 0.1, U value = 5990.0, p = 0.002). The most common new medical conditions among the high symptom load group are chronic pain (10.4%), hypertension (7.5%), and heart disease (4.5%). The high symptoms load group also has a statistically significantly higher incidence of new psychiatric conditions (7.5 vs 0.6%, Fisher’s exact test, p = 0.01) and suicidal ideas (16.4 vs 3.2%, Fisher’s exact test, p = 0.001). Additionally, they had more medical consultations (median = 3.0 vs 1.0, U value = 6787.5, p < 0.001) and days of hospitalisation (median = 0 vs 0, mean = 0.7 vs 1.0, U value = 5915.5, p = 0.007) in the past year.
The high symptom load group was less likely to have received any COVID vaccine prior to their first SARS-CoV-2 infection (4.5 vs 14.1%, Fisher’s exact test, p = 0.038) when compared to the low symptom load group, but the two groups were similar in terms of the proportion of moderate to severe/critical severity of the subjects’ COVID infection during the acute phase (34.3 vs 28.2%, Pearson’s chi-square = 0.84, p = 0.43) and whether they had single or multiple COVID infections (22.4 vs 27.6%, Pearson’s chi-square = 0.65, p = 0.51).
A multivariable logistic regression performed using age, gender, ethnicity, tertiary education, pre-pandemic Deprivation Index (log-transformed), number of pre-pandemic medical comorbidities, presence of pre-pandemic psychiatric diagnosis, receipt of COVID vaccination prior to first infection, severity of index COVID infection and single or multiple infections as predictors showed that only the pre-pandemic Deprivation Index (adjusted odd ratio = 1.55, 95% CI = 1.04–2.31, p = 0.032) and receipt of any COVID vaccination prior to first infection (adjusted odd ratio = 0.26, 95% CI = 0.07–0.92, p = 0.037) were statistically significant predictors for the high symptom load group. These two factors also predicted the count of chronic post-COVID neuropsychiatric symptoms of the subjects in a generalised negative binomial regression model using the same variables (see Supplementary material ).
Network analysis and symptom clustering
Our network model identified three distinct clusters/communities: (1) an anxiety-depression cluster containing symptoms of anxiety, insomnia, loss of interest or pleasure, depression and PTSD; (2) a cognitive complaint-fatigue cluster containing fatigue, inability to concentrate, memory problems and daytime sleepiness; and (3) a dizziness-headache cluster (Fig. 2 ). The r_com of the network was 0.68, indicating our network model likely contained discrete clusters and that the walktrap algorithm had reliably detected them.

Fat: fatigue, DSl daytime sleepiness, Mem memory problems, Con Inability to concentrate, Anx feeling anxious, Ins insomnia, Dep feeling depressed, Int loss of interest or pleasure, PTS COVID-related post-traumatic stress symptoms, Diz dizziness, Hed headache. The colour of the node represents the cluster they belong to.
Multivariable negative binomial regression models using the same predictors as our logistic regression above suggested that the pre-pandemic Deprivation index (log-transformed) positively predicts the number of chronic symptoms in both the anxiety-depression (b = 0.40, p = 0.0002) and cognitive complaint-fatigue clusters (b = 0.23, p = 0.025), but receipt of any COVID vaccination before the index infection negatively predicts only the number of symptoms from the cognitive complaint-fatigue cluster (b = −0.79, p = 0.0018) and not that of the anxiety-depression cluster (b = −0.39, p = 0.28).
To the best of our knowledge, our study is the first that examines chronic neuropsychiatric symptoms persisting beyond one year after the first SARS-CoV-2 infection using (i) non-COVID control data to define a threshold for high/low symptom load and (ii) network analysis to explore the structure of such symptoms, as well as the clinical and socioeconomic risk factors of symptom clusters.
Higher levels of fatigue and worse performance in neurocognitive tasks among post-COVID subjects
The post-COVID group had a higher level of fatigue than the matched control group after more than one year from the index infection, a finding which was not explained by depression, anxiety, PTS, or insomnia. This result echoes existing evidence that fatigue is one of the most reported PACS symptoms in the post-infection era [ 23 ], with the additional implication that fatigue may be more persistent than mood, anxiety, sleep or PTS symptoms among post-COVID patients. The post-COVID group also performed worse than the matched control group in the DSST and alternate finger-tapping tests. The DSST is a nonspecific psychomotor speed test involving multiple domains, and is sensitive in detecting cognitive dysfunction [ 24 ]. The alternate finger-tapping task is also a psychomotor speed test, though one that requires less cognitive processing. In the absence of any impairment in the subjects’ attention and working memory task performance, we are unable to pinpoint the specific deficient neurocognitive domain(s) behind the psychomotor speed impairment among the post-COVID group.
Increase in medical diagnoses and medical resource utilisation among post-COVID subjects
Post-COVID subjects had an increase in medical diagnoses since the COVID pandemic began, and showed an increase in hospitalisation in the past 1 year. This is consistent with other reports suggesting that there has been an increase in the incidence of some medical conditions after SARS-CoV-2 infection [ 9 ]. The post-COVID group did not show an increase in post-COVID psychiatric diagnoses and new suicidal ideas, however. This suggests that, as a group, there is no evidence of clinically concerning mental health deterioration after infection, despite an increase in new diagnoses of physical conditions. The socioeconomic status of post-COVID subjects as compared to the matched control group did not worsen since the COVID pandemic began, and the HRQoL of both groups were comparable. Overall, these results reflect that, as a group, there has been some change in the health status of post-COVID subjects, even though this did not have a significant impact on their social and vocational functioning and HRQoL.
Post-COVID subjects with multiple neuropsychiatric complaints had poorer mental health and HRQoL
If we look at the comparison between those with a high load of persistent neuropsychiatric symptoms and those with a low load, however, the two groups have pervasively different post-COVID health trajectories despite similar pre-COVID health. This is clearly reflected by the new incidence of medical and psychiatric diagnoses, the emergence of suicidal ideation, increased medical consultations and hospitalisations and poor current mental health and worse current HRQoL of the post-COVID group, in the absence of significant pre-COVID health and socioeconomic discrepancies as compared to the matched control group. While we cannot tell the direction of any potential causal relationship between the neuropsychiatric and other aspects of health based on our data, given that this relationship may be bidirectional, or the two may share similar pathophysiology, the bottom line is that the presence of multiple persistent post-COVID neuropsychiatric complaints reflected quantifiable and clinically relevant mental health distress. Notably, however, cognitive performance did not differ between the high and low symptom load groups. This can reflect the relationship between cognitive impairment and chronic post-COVID neuropsychiatric symptoms loading is non-linear, or the subjective cognitive complaints do not reflect objective impairment. Yet, it could also have been a result of the limitations of the tools used. For example, because the cognitive tasks were completed via a mobile phone app in an uncontrolled environment, this may have increased the variance in performance. The range of cognitive functions that our test panels could cover was also limited.
Lack of vaccination and pre-pandemic material deprivation predicts high number of chronic neuropsychiatric complaints but not index infection severity
Two of our three hypothesised risk factors, namely vaccination status before first COVID infection and pre-pandemic level of material deprivation as measured by the Deprivation Index, were found to be predictive factors of a high load of persistent neuropsychiatric symptoms. While previous studies have reported that COVID vaccinations reduce PACS [ 10 ], our study is the first to date that demonstrates that any COVID vaccination before infection reduces the risk of chronic neuropsychiatric symptoms even more than one year after infection, with this protective effect not being one that is mediated through reducing symptom severity or protection against re-infection. Thus, it is possible that vaccination reduces the dysregulated response of the immune system during SARS-CoV-2 infection, which is hypothesised to be the underlying pathophysiology of PACS. In this way, our findings highlight a further public health benefit of COVID vaccinations beyond reducing short-term morbidity and mortality.
Our results also suggest that socioeconomic factors cannot be overlooked when we are considering persistent post-COVID neuropsychiatric complaints. Material deprivation has been demonstrated to be a common contributing factor to mental health distress at the population level (Chung et al., 2021). In the context of the COVID pandemic, the association of poor COVID outcomes with health inequalities has been a recurrent theme [ 25 , 26 ]. It is, therefore, not surprising that material deprivation was found to predict chronic post-COVID neuropsychiatric symptoms. While other studies have shown similar results, the limitations in the designs of such studies, namely in terms of the potential for reverse causality, have made it difficult to draw such conclusions straightforwardly from their results. A study from Hong Kong, for example, reported financial worry as one of the predictors of post-COVID mental health trajectory [ 27 ]. Because they only measured the subjects’ evaluation of their financial situation post-COVID, however, there is difficulty determining the direction of causality given that a self-reported concern about financial status can be secondary to and a result of poor mental and physical health. A US-based study found that life stressors post-COVID are associated with neuropsychiatric outcomes 12 months post-infection [ 28 ], but the causal direction of this association is again unclear. To minimise concerns regarding reverse causality in our study, we collected pre-pandemic Deprivation Index data.
Contrary to our hypothesis, the severity of the index infection did not predict whether there would be a high or low load of chronic neuropsychiatric symptoms post-COVID. Available evidence on the ability of infection severity to predict PACS has not been consistent [ 27 , 29 , 30 , 31 , 32 ]. There is convergent evidence, however, that persistent PACS can occur in individuals with mild infections.
Embracing the heterogeneity among persistent neuropsychiatric complaints
Our network analysis suggested that the common chronic post-COVID neuropsychiatric symptoms can be grouped into two major (anxiety-depression and cognitive complaint-fatigue) and one minor (headache-dizziness) clusters, a finding which supports our hypothesis that such symptoms form clusters. These clusters suggest that there could be different sub-syndromes or even disorders under the umbrella term of persistent neuropsychiatric complaints.
We also found that socioeconomic disadvantage increased the symptom load of both major clusters, but that vaccination only significantly decreased the symptom load of the cognitive complaint-fatigue cluster. This difference in how predictive the factors were gives additional support to the idea that neuropsychiatric symptoms can be further categorised into subgroups, as different sub-syndromes may have different underlying risk factors and mechanisms.
Previous studies have also used clustering algorithms to categorise individuals with PACS into subgroups [ 33 , 31 ]. These algorithms usually use a mix of self-reported symptoms, assessment results, subject demographics and clinical factors to perform the clustering, whereas our approach is to first identify the clustering of symptoms before we examine the unique, associated factors of the discovered clusters. We argue that our approach is clearer phenomenologically because it reveals the relationship among symptoms independent of confounding sociodemographic factors. The key problem with any clustering result, however, is its generalisability. Although we have conducted extra bootstrapping procedures to demonstrate the stability of our clustering results, the further replication of these results using an independent cohort is important to support the generalisability of the clustering. To the best of our knowledge, Peter et al.’s study (Peter et al., 2022) is relatively comparable to ours in terms of study approach. Despite substantial differences in sampling, measurement and statistical tools employed, the results of their clustering analysis were largely consistent with ours: they found a cluster consisting of headache and dizziness, and another consisting of sleep, anxiety and depression.
Strengths and limitations
The key strength of this study is that it was conducted in accordance with a pre-registered, open-access protocol with pre-determined hypotheses. Another strength is that our assessment and analysis covered comprehensive demographic, clinical and socioeconomic factors, as well as symptoms and cognitive measures. The first and the key limitation of this study is the use of the convenient sampling method, which limits the certainty of any epidemiological inference. The second major limitation is the cross-sectional design of the study. While we used the pre-COVID socioeconomic and health status of the subjects for case-control matching and regression analysis, so as to avoid bias introduced by changes in their physical and mental health due to COVID, the pre-COVID socioeconomic and health status data were based on recall, and thus may be affected by recall bias. The modest sample size also limits statistical power. The third limitation is that the infection status of the subjects was based on self-report and was not verified by our own testing, which could have affected the reliability of the data. However, since Hong Kong implemented a ‘zero-COVID’ policy with very stringent surveillance prior to the Omicron wave in early 2022, the subjects’ understanding of their infection status is likely accurate. The fourth limitation is that we relied on self-reported checklists and symptom scales only, and did not conduct clinical interviews or use clinician-rated instruments. Lastly, we did not correct for multiple comparisons in our statistical tests, which increases the risk of false positive results. While using pre-registered outcome measures can partially mitigate the problem of false positivity, the evidence should only be regarded as preliminary.
Conclusions
Our study suggests that the lack of COVID vaccination and a higher level of material deprivation before the COVID pandemic predicts a higher load of chronic post-COVID neuropsychiatric symptoms that persists for more than one year post-infection. This highlights the complex interplay of biological and socioeconomic factors that contribute to chronic post-COVID neuropsychiatric symptoms. Our analysis also suggests heterogeneity among chronic post-COVID neuropsychiatric symptoms, with two major symptom clusters (anxiety-depression and cognitive complaint-fatigue) and one minor cluster (headache-dizziness). Further study into chronic neuropsychiatric sequelae should take into account the heterogeneity and complexity of its phenomenology and aetiology.
Data availability
The data that support the findings of this study will be openly available after the paper is published.
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med [Internet]. 2021;27:601–15.
Article CAS PubMed Google Scholar
White-Dzuro G, Gibson LE, Zazzeron L, White-Dzuro C, Sullivan Z, Diiorio DA, et al. Multisystem effects of COVID-19: a concise review for practitioners. Postgraduate Medicine [Internet]. 2021;133:20–7.
Article PubMed Google Scholar
Baillie JK, Lone NI, Jones S, Shaw A, Hairsine B, Kurasz C, et al. Multiorgan MRI findings after hospitalisation with COVID-19 in the UK (C-MORE): a prospective, multicentre, observational cohort study. The Lancet Respiratory Medicine [Internet]. 2023;11:1003–19.
Article Google Scholar
Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re’em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine [Internet]. 2021;38:101019.
Taquet M, Sillett R, Zhu L, Mendel J, Camplisson I, Dercon Q, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. 2022;9:815–27.
Article PubMed PubMed Central Google Scholar
Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604:697–707.
Article CAS PubMed PubMed Central Google Scholar
Besteher B, Machnik M, Troll M, Toepffer A, Zerekidze A, Rocktäschel T, et al. Larger gray matter volumes in neuropsychiatric long-COVID syndrome. Psychiatry Res. 2022;317:114836.
Besteher B, Rocktäschel T, Garza AP, Machnik M, Ballez J, Helbing DL, et al. Cortical thickness alterations and systemic inflammation define long-COVID patients with cognitive impairment. Brain Behav Immun. 2024;116:175–84.
Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21:133–46.
Tsampasian V, Elghazaly H, Chattopadhyay R, Debski M, Naing TKP, Garg P, et al. Risk factors associated with post-COVID-19 condition: a systematic review and meta-analysis. JAMA Intern Med. 2023;183:566–80.
Wong SC, Au AKW, Lo JYC, Ho PL, Hung IFN, To KKW, et al. Evolution and control of COVID-19 epidemic in Hong Kong. Viruses. 2022;14:2519.
Chung RYN, Marmot M, Mak JKL, Gordon D, Chan D, Chung GKK, et al. Deprivation is associated with anxiety and stress. A population-based longitudinal household survey among Chinese adults in Hong Kong. J Epidemiol Community Health. 2021;75:335–42.
Saunders P, Wong H, Wong WP. Deprivation and poverty in Hong Kong. Soc Policy Admin. 2014;48:556–75.
Wu KK, Chan KS. The development of the Chinese version of impact of event scale–revised (CIES-R). Soc Psychiatry Psychiatr Epidemiol. 2003;38:94–8.
Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–8.
Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, et al. Development of a fatigue scale. J Psychosomatic Res. 1993;37:147–53.
Article CAS Google Scholar
Armstrong T, Bull F. Development of the World Health Organization global physical activity questionnaire (GPAQ). J Public Health. 2006;14:66–70.
The Whoqol Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28:551–8.
McWhirter L, Smyth H, Hoeritzauer I, Couturier A, Stone J, Carson AJ. What is brain fog? J Neurol Neurosurg Psychiatry. 2023;94:321.
Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res. 2018;50:195–212.
van Borkulo CD, Borsboom D, Epskamp S, Blanken TF, Boschloo L, Schoevers RA, et al. A new method for constructing networks from binary data. Sci Rep. 2014;4:5918
Shizuka D, Farine DR. Measuring the robustness of network community structure using assortativity. Animal Behaviour. 2016;112:237–46.
Peter RS, Nieters A, Kräusslich HG, Brockmann SO, Göpel S, Kindle G, et al. Post-acute sequelae of covid-19 six to 12 months after infection: population based study. BMJ. 2022;379:e071050.
Jaeger J. Digit symbol substitution test. J Clin Psychopharmacol. 2018;38:513–9.
Chung RYN, Chung GKK, Marmot M, Allen J, Chan D, Goldblatt P, et al. COVID-19 related health inequality exists even in a city where disease incidence is relatively low: a telephone survey in Hong Kong. J Epidemiol Community Health. 2021;75:616–23.
Woodward M, Peters SAE, Harris K. Social deprivation as a risk factor for COVID-19 mortality among women and men in the UK Biobank: nature of risk and context suggests that social interventions are essential to mitigate the effects of future pandemics. J Epidemiol Community Health. 2021;75:1050–5.
Leung ONW, Chiu NKH, Wong SYS, Cuijpers P, Alonso J, Chan PKS, et al. Dimensional structure of one-year post-COVID-19 neuropsychiatric and somatic sequelae and association with role impairment. Sci Rep. 2023;13:12205.
Frontera JA, Sabadia S, Yang D, de Havenon A, Yaghi S, Lewis A, et al. Life stressors significantly impact long-term outcomes and post-acute symptoms 12-months after COVID-19 hospitalization. J Neurol Sci. 2022;443:120487.
Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. 2022;101:93–135.
Elmazny A, Magdy R, Hussein M, Elsebaie EH, Ali SH, Abdel Fattah AM, et al. Neuropsychiatric post-acute sequelae of COVID-19: prevalence, severity, and impact of vaccination. Eur Arch Psychiatry Clin Neurosci. 2023;273:1349–58. https://doi.org/10.1007/s00406-023-01557-2
Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med. 2021;9:1275–87.
Townsend L, Dyer AH, Jones K, Dunne J, Mooney A, Gaffney F, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE. 2020;15:e0240784.
Zhao Y, Shi L, Jiang Z, Zeng N, Mei H, Lu Y, et al. The phenotype and prediction of long-term physical, mental and cognitive COVID-19 sequelae 20 months after recovery, a community-based cohort study in China. Mol Psychiatry. 2023;28:1793–801.
Download references
Acknowledgements
We thank Ms. Janet Tse for her logistical support in conducting the research. We thank Ms. Daisy Cheung for her very helpful comments and suggestions on the manuscript. This work was supported by the Research Grant Council (SWHC, grant number C4061-21G) and the Health Bureau, Hong Kong SAR (RNYC and YKW, grant number COVID1903002).
Author information
Authors and affiliations.
Department of Psychiatry, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, China
Steven Wai Ho Chau, Timothy Mitchell Chue, Rachel Ngan Yin Chan, Yee Lok Lai, Yaping Liu, Joey Wing Yan Chan & Yun Kwok Wing
Li Chiu Kong Family Sleep Assessment Unit, Department of Psychiatry, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, China
Steven Wai Ho Chau, Rachel Ngan Yin Chan, Joey Wing Yan Chan & Yun Kwok Wing
Department of Social Work and Social Administration, Faculty of Social Science, The University of Hong Kong, Hong Kong, China
Paul W. C. Wong
Department of Psychology, Faculty of Social Science, The University of Hong Kong, Hong Kong, China
Shirley Xin Li
Center for Sleep and Circadian Medicine, The Affiliated Brain Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China
Department of Microbiology, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, China
Paul Kay-sheung Chan & Christopher K. C. Lai
Division of Neurology, Department of Medicine and Therapeutics, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, China
Thomas W. H. Leung
You can also search for this author in PubMed Google Scholar
Contributions
SWHC, RNYC, PWCW and YKW contributed to the design of the study. SWHC, RNYC, PWCW, SXL, YL, JWYC, PK-sC, CKCL, TWHL and YKW contributed to the funding acquisition. SWHC, SXL, RNYC and YL contributed to the design of the assessment material. SWHC, TMC and YLL performed data analysis and wrote the first draft of the manuscript. All authors critically reviewed and approved the final manuscript.
Corresponding author
Correspondence to Steven Wai Ho Chau .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary materials, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Chau, S.W.H., Chue, T.M., Chan, R.N.Y. et al. Chronic post-COVID neuropsychiatric symptoms persisting beyond one year from infection: a case-control study and network analysis. Transl Psychiatry 14 , 261 (2024). https://doi.org/10.1038/s41398-024-02978-w
Download citation
Received : 31 October 2023
Revised : 18 May 2024
Accepted : 10 June 2024
Published : 19 June 2024
DOI : https://doi.org/10.1038/s41398-024-02978-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Introduction
- Conclusions
- Article Information
Contributing studies for clinically elevated depression symptoms are presented in order of largest to smallest prevalence rate. Square data markers represent prevalence rates, with lines around the marker indicating 95% CIs. The diamond data marker represents the overall effect size based on included studies.
Contributing studies for clinically elevated anxiety symptoms are presented in order of largest to smallest prevalence rate. Square data markers represent prevalence rates, with lines around the marker indicating 95% CIs. The diamond data marker represents the overall effect size based on included studies.
eTable 1. Example Search Strategy from Medline
eTable 2. Study Quality Evaluation Criteria
eTable 3. Quality Assessment of Studies Included
eTable 4. Sensitivity analysis excluding low quality studies (score=2) for moderators of the prevalence of clinically elevated depressive symptoms in children and adolescence during COVID-19
eTable 5. Sensitivity analysis excluding low quality studies (score=2) for moderators of the prevalence of clinically elevated anxiety symptoms in children and adolescence during COVID-19
eFigure 1. PRISMA diagram of review search strategy
eFigure 2. Funnel plot for studies included in the clinically elevated depressive symptoms
eFigure 3. Funnel plot for studies included in the clinically elevated anxiety symptoms
- Pediatric Depression and Anxiety Doubled During the Pandemic JAMA News From the JAMA Network October 5, 2021 Anita Slomski
- Guidelines Synopsis: Screening for Anxiety in Adolescent and Adult Women JAMA JAMA Clinical Guidelines Synopsis March 8, 2022 This JAMA Clinical Guidelines Synopsis summarizes the 2020 Women’s Preventive Services Initiative recommendation on screening for anxiety in adolescent and adult women. Tiffany I. Leung, MD, MPH; Adam S. Cifu, MD; Wei Wei Lee, MD, MPH
- Addressing the Global Crisis of Child and Adolescent Mental Health JAMA Pediatrics Editorial November 1, 2021 Tami D. Benton, MD; Rhonda C. Boyd, PhD; Wanjikũ F.M. Njoroge, MD
- Effect of the COVID-19 pandemic on Adolescents With Eating Disorders JAMA Pediatrics Comment & Response February 1, 2022 Thonmoy Dey, BSc; Zachariah John Mansell, BSc; Jasmin Ranu, BSc
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
Racine N , McArthur BA , Cooke JE , Eirich R , Zhu J , Madigan S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19 : A Meta-analysis . JAMA Pediatr. 2021;175(11):1142–1150. doi:10.1001/jamapediatrics.2021.2482
Manage citations:
© 2024
- Permissions
Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19 : A Meta-analysis
- 1 Department of Psychology, University of Calgary, Calgary, Alberta, Canada
- 2 Alberta Children’s Hospital Research Institute, Calgary, Alberta, Canada
- Editorial Addressing the Global Crisis of Child and Adolescent Mental Health Tami D. Benton, MD; Rhonda C. Boyd, PhD; Wanjikũ F.M. Njoroge, MD JAMA Pediatrics
- News From the JAMA Network Pediatric Depression and Anxiety Doubled During the Pandemic Anita Slomski JAMA
- JAMA Clinical Guidelines Synopsis Guidelines Synopsis: Screening for Anxiety in Adolescent and Adult Women Tiffany I. Leung, MD, MPH; Adam S. Cifu, MD; Wei Wei Lee, MD, MPH JAMA
- Comment & Response Effect of the COVID-19 pandemic on Adolescents With Eating Disorders Thonmoy Dey, BSc; Zachariah John Mansell, BSc; Jasmin Ranu, BSc JAMA Pediatrics
Question What is the global prevalence of clinically elevated child and adolescent anxiety and depression symptoms during COVID-19?
Findings In this meta-analysis of 29 studies including 80 879 youth globally, the pooled prevalence estimates of clinically elevated child and adolescent depression and anxiety were 25.2% and 20.5%, respectively. The prevalence of depression and anxiety symptoms during COVID-19 have doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls.
Meaning The global estimates of child and adolescent mental illness observed in the first year of the COVID-19 pandemic in this study indicate that the prevalence has significantly increased, remains high, and therefore warrants attention for mental health recovery planning.
Importance Emerging research suggests that the global prevalence of child and adolescent mental illness has increased considerably during COVID-19. However, substantial variability in prevalence rates have been reported across the literature.
Objective To ascertain more precise estimates of the global prevalence of child and adolescent clinically elevated depression and anxiety symptoms during COVID-19; to compare these rates with prepandemic estimates; and to examine whether demographic (eg, age, sex), geographical (ie, global region), or methodological (eg, pandemic data collection time point, informant of mental illness, study quality) factors explained variation in prevalence rates across studies.
Data Sources Four databases were searched (PsycInfo, Embase, MEDLINE, and Cochrane Central Register of Controlled Trials) from January 1, 2020, to February 16, 2021, and unpublished studies were searched in PsycArXiv on March 8, 2021, for studies reporting on child/adolescent depression and anxiety symptoms. The search strategy combined search terms from 3 themes: (1) mental illness (including depression and anxiety), (2) COVID-19, and (3) children and adolescents (age ≤18 years). For PsycArXiv , the key terms COVID-19 , mental health , and child/adolescent were used.
Study Selection Studies were included if they were published in English, had quantitative data, and reported prevalence of clinically elevated depression or anxiety in youth (age ≤18 years).
Data Extraction and Synthesis A total of 3094 nonduplicate titles/abstracts were retrieved, and 136 full-text articles were reviewed. Data were analyzed from March 8 to 22, 2021.
Main Outcomes and Measures Prevalence rates of clinically elevated depression and anxiety symptoms in youth.
Results Random-effect meta-analyses were conducted. Twenty-nine studies including 80 879 participants met full inclusion criteria. Pooled prevalence estimates of clinically elevated depression and anxiety symptoms were 25.2% (95% CI, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively. Moderator analyses revealed that the prevalence of clinically elevated depression and anxiety symptoms were higher in studies collected later in the pandemic and in girls. Depression symptoms were higher in older children.
Conclusions and Relevance Pooled estimates obtained in the first year of the COVID-19 pandemic suggest that 1 in 4 youth globally are experiencing clinically elevated depression symptoms, while 1 in 5 youth are experiencing clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double of prepandemic estimates. An influx of mental health care utilization is expected, and allocation of resources to address child and adolescent mental health concerns are essential.
Prior to the COVID-19 pandemic, rates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% 1 and 12.9%, 2 respectively. Since COVID-19 was declared an international public health emergency, youth around the world have experienced dramatic disruptions to their everyday lives. 3 Youth are enduring pervasive social isolation and missed milestones, along with school closures, quarantine orders, increased family stress, and decreased peer interactions, all potential precipitants of psychological distress and mental health difficulties in youth. 4 - 7 Indeed, in both cross-sectional 8 , 9 and longitudinal studies 10 , 11 amassed to date, the prevalence of youth mental illness appears to have increased during the COVID-19 pandemic. 3 However, data collected vary considerably. Specifically, ranges from 2.2% 12 to 63.8% 13 and 1.8% 12 to 49.5% 13 for clinically elevated depression and anxiety symptoms, respectively. As governments and policy makers deploy and implement recovery plans, ascertaining precise estimates of the burden of mental illness for youth are urgently needed to inform service deployment and resource allocation.
Depression and generalized anxiety are 2 of the most common mental health concerns in youth. 14 Depressive symptoms, which include feelings of sadness, loss of interest and pleasure in activities, as well as disruption to regulatory functions such as sleep and appetite, 15 could be elevated during the pandemic as a result of social isolation due to school closures and physical distancing requirements. 6 Generalized anxiety symptoms in youth manifest as uncontrollable worry, fear, and hyperarousal. 15 Uncertainty, disruptions in daily routines, and concerns for the health and well-being of family and loved ones during the COVID-19 pandemic are likely associated with increases in generalized anxiety in youth. 16
When heterogeneity is observed across studies, as is the case with youth mental illness during COVID-19, it often points to the need to examine demographic, geographical, and methodological moderators. Moderator analyses can determine for whom and under what circumstances prevalence is higher vs lower. With regard to demographic factors, prevalence rates of mental illness both prior to and during the COVID-19 pandemic are differentially reported across child age and sex, with girls 17 , 18 and older children 17 , 19 being at greater risk for internalizing disorders. Studies have also shown that youth living in regions that experienced greater disease burden 2 and urban areas 20 had greater mental illness severity. Methodological characteristics of studies also have the potential to influence the estimated prevalence rates. For example, studies of poorer methodological quality may be more likely to overestimate prevalence rates. 21 The symptom reporter (ie, child vs parent) may also contribute to variability in the prevalence of mental illness across studies. Indeed, previous research prior to the pandemic has demonstrated that child and parent reports of internalizing symptoms vary, 22 with children/adolescents reporting more internalizing symptoms than parents. 23 Lastly, it is important to consider the role of data collection timing on potential prevalence rates. While feelings of stress and overwhelm may have been greater in the early months of the pandemic compared with later, 24 extended social isolation and school closures may have exerted mental health concerns.
Although a narrative systematic review of 6 studies early in the pandemic was conducted, 8 to our knowledge, no meta-analysis of prevalence rates of child and adolescent mental illness during the pandemic has been undertaken. In the current study, we conducted a meta-analysis of the global prevalence of clinically elevated symptoms of depression and anxiety (ie, exceeding a clinical cutoff score on a validated measure or falling in the moderate to severe symptom range of anxiety and depression) in youth during the first year of the COVID-19 pandemic. While research has documented a worsening of symptoms for children and youth with a wide range of anxiety disorders, 25 including social anxiety, 26 clinically elevated symptoms of generalized anxiety are the focus of the current meta-analysis. In addition to deriving pooled prevalence estimates, we examined demographic, geographical, and methodological factors that may explain between-study differences. Given that there have been several precipitants of psychological distress for youth during COVID-19, we hypothesized that pooled prevalence rates would be higher compared with prepandemic estimates. We also hypothesized that child mental illness would be higher among studies with older children, a higher percentage of female individuals, studies conducted later in the pandemic, and that higher-quality studies would have lower prevalence rates.
This systematic review was registered as a protocol with PROSPERO (CRD42020184903) and the Preferred Reporting Items for Systematic Reviews and Meta-analyses ( PRISMA ) reporting guideline was followed. 27 Ethics review was not required for the study. Electronic searches were conducted in collaboration with a health sciences librarian in PsycInfo, Cochrane Central Register of Controlled Trials (CENTRAL), Embase, and MEDLINE from inception to February 16, 2021. The search strategy (eTable 1 in the Supplement ) combined search terms from 3 themes: (1) mental illness (including depression and anxiety), (2) COVID-19, and (3) children and adolescents (age ≤18 years). Both database and subject headings were used to search keywords. As a result of the rapidly evolving nature of research during the COVID-19 pandemic, we also searched a repository of unpublished preprints, PsycArXiv . The key terms COVID-19 , mental health , and child/adolescent were used on March 8, 2021, and yielded 38 studies of which 1 met inclusion criteria.
The following inclusion criteria were applied: (1) sample was drawn from a general population; (2) proportion of individuals meeting clinical cutoff scores or falling in the moderate to severe symptom range of anxiety or depression as predetermined by validated self-report measures were provided; (3) data were collected during COVID-19; (4) participants were 18 years or younger; (5) study was empirical; and (6) studies were written in English. Samples of participants who may be affected differently from a mental health perspective during COVID-19 were excluded (eg, children with preexisting psychiatric diagnoses, children with chronic illnesses, children diagnosed or suspected of having COVID-19). We also excluded case studies and qualitative analyses.
Five (N.R., B.A.M., J.E.C., R.E. and J.Z.) authors used Covidence software (Covidence Inc) to review all abstracts and to determine if the study met criteria for inclusion. Twenty percent of abstracts reviewed for inclusion were double-coded, and the mean random agreement probability was 0.89; disagreements were resolved via consensus with the first author (N.R.). Two authors (N.R. and B.A.M.) reviewed full-text articles to determine if they met all inclusion criteria and the percent agreement was 0.80; discrepancies were resolved via consensus.
When studies met inclusion criteria, prevalence rates for anxiety and depression were extracted, as well as potential moderators. When more than 1 wave of data was provided, the wave with the largest sample size was selected. For 1 study in which both parent and youth reports were provided, 26 the youth report was selected, given research that they are the reliable informants of their own behavior. 28 The following moderators were extracted: (1) study quality (see the next subsection); (2) participant age (continuously as a mean); (3) sex (% female in a sample); (4) geographical region (eg, East Asia, Europe, North America), (5) informant (child, parent), (6) month in 2020 when data were collected (range, 1-12). Data from all studies were extracted by 1 coder and the first author (N.R.). Discrepancies were resolved via consensus.
Adapted from the National Institute of Health Quality Assessment Tool for Observation Cohort and Cross-Sectional Studies, a short 5-item questionnaire was used (eTable 2 in the Supplement ). 29 Studies were given a score of 0 (no) or 1 (yes) for each of the 5 criteria (validated measure; peer-reviewed, response rate ≥50%, objective assessment, sufficient exposure time) and summed to give a total score of 5. When information was unclear or not provided by the study authors, it was marked as 0 (no).
All included studies are from independent samples. Comprehensive Meta-Analysis version 3.0 (Biostat) software was used for data analysis. Pooled prevalence estimates with associated 95% confidence intervals around the estimate were computed. We weighted pooled prevalence estimates by the weight of the inverse of their variance, which gives greater weight to large sample sizes.
We used random-effects models to reflect the variations observed across studies and assessed between-study heterogeneity using the Q and I 2 statistics. Pooled prevalence is reported as an event rate (ie, 0.30) but interpreted as prevalence (ie, 30.0%). Significant Q statistics and I 2 values more than 75% suggest moderator analyses should be explored. 30 As recommended by Bornstein et al, 30 we examined categorical moderators when k of 10 or higher and a minimum cell size of k more than 3 were available. A P value of .05 was considered statistically significant. For continuous moderators, random-effect meta-regression analyses were conducted. Publication bias was examined using the Egger test 31 and by inspecting funnel plots for symmetry.
Our electronic search yielded 3094 nonduplicate records (eFigure 1 in the Supplement ). Based on the abstract review, a total of 136 full-text articles were retrieved to examine against inclusion criteria, and 29 nonoverlapping studies 10 , 12 , 13 , 17 , 19 , 20 , 26 , 32 - 53 met full inclusion criteria.
A total of 29 studies were included in the meta-analyses, of which 26 had youth symptom reports and 3 studies 39 , 42 , 48 had parent reports of child symptoms. As outlined in Table 1 , across all 29 studies, 80 879 participants were included, of which the mean (SD) perecentage of female individuals was 52.7% (12.3%), and the mean age was 13.0 years (range, 4.1-17.6 years). All studies provided binary reports of sex or gender. Sixteen studies (55.2%) were from East Asia, 4 were from Europe (13.8%), 6 were from North America (20.7%), 2 were from Central America and South America (6.9%), and 1 study was from the Middle East (3.4%). Eight studies (27.6%) reported having racial or ethnic minority participants with the mean across studies being 36.9%. Examining study quality, the mean score was 3.10 (range, 2-4; eTable 3 in the Supplement ).
The pooled prevalence from a random-effects meta-analysis of 26 studies revealed a pooled prevalence rate of 0.25 (95% CI, 0.21-0.30; Figure 1 ) or 25.2%. The funnel plot was symmetrical (eFigure 2 in the Supplement ); however, the Egger test was statistically significant (intercept, −9.5; 95% CI, −18.4 to −0.48; P = .02). The between-study heterogeneity statistic was significant ( Q = 4675.91; P < .001; I 2 = 99.47). Significant moderators are reported below, and all moderator analyses are presented in Table 2 .
As the number of months in the year increased, so too did the prevalence of depressive symptoms ( b = 0.26; 95% CI, 0.06-0.46). Prevalence rates were higher as child age increased ( b = 0.08; 95% CI, 0.01-0.15), and as the percentage of female individuals ( b = 0.03; 95% CI, 0.01-0.05) in samples increased. Sensitivity analyses removing low-quality studies were conducted (ie, scores of 2) 32 , 43 (eTable 4 in the Supplement ). Moderators remained significant, except for age, which became nonsignificant ( b = 0.06; 95% CI, −0.02 to 0.13; P = .14).
The overall pooled prevalence rate across 25 studies for elevated anxiety was 0.21 (95% CI, 0.17-0.24; Figure 2 ) or 20.5%. The funnel plot was symmetrical (eFigure 3 in the Supplement ) and the Egger test was nonsignificant (intercept, −6.24; 95% CI, −14.10 to 1.62; P = .06). The heterogeneity statistic was significant ( Q = 3300.17; P < .001; I 2 = 99.27). Significant moderators are reported below, and all moderator analyses are presented in Table 3 .
As the number of months in the year increased, so too did the prevalence of anxiety symptoms ( b = 0.27; 95% CI, 0.10-0.44). Prevalence rates of clinically elevated anxiety was higher as the percentage of female individuals in the sample increased ( b = 0.04; 95% CI, 0.01-0.07) and also higher in European countries ( k = 4; rate = 0.34; 95% CI, 0.23-0.46; P = .01) compared with East Asian countries ( k = 14; rate = 0.17; 95% CI, 0.13-0.21; P < .001). Lastly, the prevalence of clinically elevated anxiety was higher in studies deemed to have poorer quality ( k = 21; rate = 0.22; 95% CI, 0.18-0.27; P < .001) compared with studies with better study quality scores ( k = 4; rate = 0.12; 95% CI, 0.07-0.20; P < .001). Sensitivity analyses removing low quality studies (ie, scores of 2) 32 , 43 yielded the same pattern of results (eTable 5 in the Supplement ).
The current meta-analysis provides a timely estimate of clinically elevated depression and generalized anxiety symptoms globally among youth during the COVID-19 pandemic. Across 29 samples and 80 879 youth, the pooled prevalence of clinically elevated depression and anxiety symptoms was 25.2% and 20.5%, respectively. Thus, 1 in 4 youth globally are experiencing clinically elevated depression symptoms, while 1 in 5 youth are experiencing clinically elevated anxiety symptoms. A comparison of these findings to prepandemic estimates (12.9% for depression 2 and 11.6% for anxiety 1 ) suggests that youth mental health difficulties during the COVID-19 pandemic has likely doubled.
The COVID-19 pandemic, and its associated restrictions and consequences, appear to have taken a considerable toll on youth and their psychological well-being. Loss of peer interactions, social isolation, and reduced contact with buffering supports (eg, teachers, coaches) may have precipitated these increases. 3 In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs. 54 For many children, these services were rendered unavailable owing to school closures.
As the month of data collection increased, rates of depression and anxiety increased correspondingly. One possibility is that ongoing social isolation, 6 family financial difficulties, 55 missed milestones, and school disruptions 3 are compounding over time for youth and having a cumulative association. However, longitudinal research supporting this possibility is currently scarce and urgently needed. A second possibility is that studies conducted in the earlier months of the pandemic (February to March 2020) 12 , 51 were more likely to be conducted in East Asia where self-reported prevalence of mental health symptoms tends to be lower. 56 Longitudinal trajectory research on youth well-being as the pandemic progresses and in pandemic recovery phases will be needed to confirm the long-term mental health implications of the COVID-19 pandemic on youth mental illness.
Prevalence rates for anxiety varied according to study quality, with lower-quality studies yielding higher prevalence rates. It is important to note that in sensitivity analyses removing lower-quality studies, other significant moderators (ie, child sex and data collection time point) remained significant. There has been a rapid proliferation of youth mental health research during the COVID-19 pandemic; however, the rapid execution of these studies has been criticized owing to the potential for some studies to sacrifice methodological quality for methodological rigor. 21 , 57 Additionally, several studies estimating prevalence rates of mental illness during the pandemic have used nonprobability or convenience samples, which increases the likelihood of bias in reporting. 21 Studies with representative samples and/or longitudinal follow-up studies that have the potential to demonstrate changes in mental health symptoms from before to after the pandemic should be prioritized in future research.
In line with previous research on mental illness in childhood and adolescence, 58 female sex was associated with both increased depressive and anxiety symptoms. Biological susceptibility, lower baseline self-esteem, a higher likelihood of having experienced interpersonal violence, and exposure to stress associated with gender inequity may all be contributing factors. 59 Higher rates of depression in older children were observed and may be due to puberty and hormonal changes 60 in addition to the added effects of social isolation and physical distancing on older children who particularly rely on socialization with peers. 6 , 61 However, age was not a significant moderator for prevalence rates of anxiety. Although older children may be more acutely aware of the stress of their parents and the implications of the current global pandemic, younger children may be able to recognize changes to their routine, both of which may contribute to similar rates of anxiety with different underlying mechanisms.
In terms of practice implications, a routine touch point for many youth is the family physician or pediatrician’s office. Within this context, it is critical to inquire about or screen for youth mental health difficulties. Emerging research 42 suggests that in families using more routines during COVID-19, lower child depression and conduct problems are observed. Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity. Additional resources should be made available, and clinical referrals should be placed when children experience clinically elevated mental distress. At a policy level, research suggests that social isolation may contribute to and confer risk for mental health concerns. 4 , 5 As such, the closure of schools and recreational activities should be considered a last resort. 62 In addition, methods of delivering mental health resources widely to youth, such as group and individual telemental health services, need to be adapted to increase scalability, while also prioritizing equitable access across diverse populations. 63
There are some limitations to the current study. First, although the current meta-analysis includes global estimates of child and adolescent mental illness, it will be important to reexamine cross-regional differences once additional data from underrepresented countries are available. Second, most study designs were cross-sectional in nature, which precluded an examination of the long-term association of COVID-19 with child mental health over time. To determine whether clinically elevated symptoms are sustained, exacerbated, or mitigated, longitudinal studies with baseline estimates of anxiety and depression are needed. Third, few studies included racial or ethnic minority participants (27.6%), and no studies included gender-minority youth. Given that racial and ethnic minority 64 and gender-diverse youth 65 , 66 may be at increased risk for mental health difficulties during the pandemic, future work should include and focus on these groups. Finally, all studies used self- or parent-reported questionnaires to examine the prevalence of clinically elevated (ie, moderate to high) symptoms. Thus, studies using criterion standard assessments of child depression and anxiety disorders via diagnostic interviews or multimethod approaches may supplement current findings and provide further details on changes beyond generalized anxiety symptoms, such symptoms of social anxiety, separation anxiety, and panic.
Overall, this meta-analysis shows increased rates of clinically elevated anxiety and depression symptoms for youth during the COVID-19 pandemic. While this meta-analysis supports an urgent need for intervention and recovery efforts aimed at improving child and adolescent well-being, it also highlights that individual differences need to be considered when determining targets for intervention (eg, age, sex, exposure to COVID-19 stressors). Research on the long-term effect of the COVID-19 pandemic on mental health, including studies with pre– to post–COVID-19 measurement, is needed to augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth.
Corresponding Author: Sheri Madigan, PhD, RPsych, Department of Psychology University of Calgary, Calgary, AB T2N 1N4, Canada ( [email protected] ).
Accepted for Publication: May 19, 2021.
Published Online: August 9, 2021. doi:10.1001/jamapediatrics.2021.2482
Author Contributions: Drs Racine and Madigan had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Racine, Madigan.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Racine, McArthur, Eirich, Zhu, Madigan.
Critical revision of the manuscript for important intellectual content: Racine, Cooke, Eirich, Madigan.
Statistical analysis: Racine, McArthur.
Administrative, technical, or material support: Madigan.
Supervision: Racine, Madigan.
Conflict of Interest Disclosures: Dr Racine reported fellowship support from Alberta Innovates. Dr McArthur reported a postdoctoral fellowship award from the Alberta Children’s Hospital Research Institute. Ms Cooke reported graduate scholarship support from Vanier Canada and Alberta Innovates Health Solutions outside the submitted work. Ms Eirich reported graduate scholarship support from the Social Science and Humanities Research Council. No other disclosures were reported.
Additional Contributions: We acknowledge Nicole Dunnewold, MLIS (Research and Learning Librarian, Health Sciences Library, University of Calgary), for her assistance with the search strategy, for which they were not compensated outside of their salary. We also acknowledge the contribution of members of the Determinants of Child Development Laboratory at the University of Calgary, in particular, Julianna Watt, BA, and Katarina Padilla, BSc, for their contribution to data extraction, for which they were paid as research assistants.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.
High airfares to persist as travel booms, new AirAsia boss says
PUBLISHED : 24 Jun 2024 at 09:06
WRITER: Bloomberg

There’s no end in sight to the high airfares that are a mainstay of the world’s post-pandemic travel boom, according to Asia’s biggest low-cost carrier.
Travellers may see a little reprieve next year as jet fuel prices decline and the airline’s flight capacity rises, said AirAsia Aviation Chief Executive Officer Bo Lingam, who will head a new listed entity called AirAsia Group following a merger between the company’s short and long haul operations in September. But strong demand means airfares are unlikely to return to pre-pandemic levels any time soon, he said.
“My load factor is around 90% — this was unheard of pre-Covid,” Lingam, 59, said in an interview at the company’s headquarters in Sepang, Malaysia.
The global aviation industry has been transformed as the post-pandemic reopening unleashed a wave of pent-up travel demand that’s sent ticket prices surging faster than inflation in many parts of the world. At the same time, a series of supply chain constraints from aircraft delivery delays to unplanned engine maintenance has left many airlines struggling to roll out enough flights.
For AirAsia, the demand is underpinning ambitions to establish the world’s first low-cost carrier network by 2030, using its Southeast Asia bases as a hub. So far this year that’s seen it add flights to Almaty in Kazakhstan and the start of operations by its Cambodian unit. Next up will be to start flying to Nairobi, Kenya, from October.
Its further-afield routes will be serviced by Airbus SE’s new long-range A321 models, which can fly further at an economical cost. Lingam said the company intends to convert its entire 377-plane orderbook to the A321 LR models and has made a separate order for 50 XLR models.
“The cost of operating the aircraft is much cheaper — at least 25% to 30% cheaper — because it’s single aisle and you don’t need to worry about filling up 500 seats, as opposed to 240 seats,” Lingam said.
Lingam also said there will be “no changes” in the way AirAsia is run when founder Tony Fernandes moves to an advisory role following the merger and shifts his focus towards non-aviation businesses under Capital A Bhd.
While he hasn’t yet started his new role, Lingam, who has worked with Fernandes for more than three decades, said he’s already looking at his own succession plans. He intends to transfer his know-how to his two deputy CEOs, Chester Voo and Farouk Kamal over the next five years.
“I’m no spring chicken,” he said.
Other key takeaways from the interview:
- AirAsia is looking to raise at least US$400 million in debt financing and 1 billion ringgit ($212 million) through equity once its merger completes.
- The company is looking to refinance its dollar debts into ringgit, and will also seek lower interest rates once it’s removed from the Malaysian stock exchange’s financially distressed classification.
- AirAsia is in discussions to start a unit in Vietnam, adding to its presence in Malaysia, Thailand, the Philippines, Indonesia and Cambodia. The company won’t look to start units in any countries outside Southeast Asia.
RECOMMENDED
Harman building b2.8bn thai factory, pm vows to get ‘ferrari’ economy humming, india buys record amount of sunoil amid ukraine-russia price war, frenzied fundraising, sports events offer a leg up for thai tv market.

Airline profits stay stagnant in Asia-Pacific
India shuns china’s calls to resume direct flights, extra 7,000 seats per week agreed for india flights.

How bad is traffic in Dallas? One study says its only getting worse
Dallas roads are getting more congested, according to a new traffic study.
Transportation data and analytics company INRIX studied hundreds of cities around the world and found that post-COVID, traffic patterns are still adjusting , with a new midday rush hour and different peak travel times.
Traffic in Dallas has increased 12% compared to before the pandemic, according to the company’s 2023 Global Traffic Scorecard. The report ranked Dallas as the 17th most congested city in the country.
Long-distance commuting has surged across the country after the pandemic, according to a study by Stanford University researchers . On average, people who work in Dallas have added 35 miles per trip to their commutes. “Super commuting” more than 75 miles to work has increased 29% post-pandemic, the study found.
Bob Pishue, the traffic scorecard’s author and a transportation data analyst at INRIX, said Dallas doesn’t have as much traffic as other large metros, despite its large size. Toll roads and public-private partnerships give the city more ways to address transportation issues to alleviate traffic.
“Texas is always looking at interesting ways to finance and deliver infrastructure, and that is not that common in other states or areas,” Pishue said. “Dallas isn’t afraid to build.”
While the city isn’t at the top of the country’s most congested cities, Dallas drivers still face busy roads every day.
“If you’re sitting in it, it sucks,” Pishue said. “[But] for its size, it does pretty well in terms of traffic congestion and delay.”
The average driver in Dallas lost 38 hours due to congestion in 2023, a six-hour increase from 2022, costing $658 in wasted time. This was slightly below the national average of 42 hours. The value of time lost in traffic was based on the U.S. Federal Highway Administration’s 2016 guidance , which puts one hour in traffic at $17.45 after adjusting for inflation. The value takes into account a population’s average hourly income, demographics, mode of transportation, purpose of travel, distance and other factors.
Dallas’ US-80 Eastbound from I-635 to FM 548 in Forney was the 11th most congested corridor in the country, with drivers losing 66 hours due to traffic on that corridor alone. Its peak congestion is reported around 5 p.m., the study found. The Texas Department of Transportation is in the process of expanding that route from two to three lanes in each direction as the Kaufman County city ranks among the fastest growing in the country.
I-30 Westbound from St. Francis Avenue to I-345 is the city’s second busiest corridor, with an average delay of 34 hours annually for Dallas drivers. Third was North Walton Walker Blvd.
The company has published an annual report on traffic patterns for more than 15 years. The scorecard looks at nearly 1,000 cities across 37 countries to see how traffic is changing and uses anonymized data from trucking fleets, delivery vehicles, passenger vehicles, mobile apps and more.
The pandemic changed traffic patterns, but congestion is ramping back up as people return to offices. Still, Pishue sees a “new normal” on the roads. Dallas is one of many American cities experiencing a new mid-day traffic rush as work schedules are more flexible and many people work from home.
INRIX found a 23% increase in mid-day trips in the U.S. compared to before the pandemic. Almost as many trips are made nationwide at noon as at 5 p.m., the report said. Work hours and changes to the traditional workday have also affected traffic patterns. Across the country, the hours of 10 a.m. and 4 p.m. each saw a higher volume of trips than 9 a.m. and 5 p.m.
Another change has occurred in downtown trips. In Dallas, Pishue said the downtown holds only about 2% of the region’s jobs, and the pandemic deemphasized, to different degrees, downtown areas across the country as economic centers. But in 2023, the city’s downtown trip volume was up 3% and the average speed for drivers downtown was 16 mph.
The scorecard put New York City as the most congested city in the world, followed by Mexico City and London. According to the report, traffic congestion shows economic growth but also means lost time and money for commuters.
The report helps cities identify problems in transportation systems and address issues relating to traffic patterns , Pishue said.
“Those that do it best, at least right now, are looking at these post-COVID travel patterns and adjusting,” Pishue said. “That’s what it’s about, is being able to adjust more frequently.”
©2024 The Dallas Morning News. Visit dallasnews.com. Distributed by Tribune Content Agency, LLC.

We use cookies to understand how you use our site and to improve your experience. This includes personalizing content and advertising. To learn more, click here . By continuing to use our site, you accept our use of cookies, revised Privacy Policy and Terms of Service .

New to Zacks? Get started here.
Member Sign In
Don't Know Your Password?

- Zacks #1 Rank
- Zacks Industry Rank
- Zacks Sector Rank
- Equity Research
- Mutual Funds
- Mutual Fund Screener
- ETF Screener
- Earnings Calendar
- Earnings Releases
- Earnings ESP
- Earnings ESP Filter
- Stock Screener
- Premium Screens
- Basic Screens
- Thematic Screens
- Research Wizard
- Personal Finance
- Money Management
- Retirement Planning
- Tax Information
- My Portfolio
- Create Portfolio
- Style Scores
- Testimonials
- Zacks.com Tutorial
Services Overview
- Zacks Ultimate
- Zacks Investor Collection
- Zacks Premium
Investor Services
- ETF Investor
- Home Run Investor
- Income Investor
- Stocks Under $10
- Value Investor
- Top 10 Stocks
Other Services
- Method for Trading
- Zacks Confidential
Trading Services
- Black Box Trader
- Counterstrike
- Headline Trader
- Insider Trader
- Large-Cap Trader
- Options Trader
- Short Sell List
- Surprise Trader
- Alternative Energy

You are being directed to ZacksTrade, a division of LBMZ Securities and licensed broker-dealer. ZacksTrade and Zacks.com are separate companies. The web link between the two companies is not a solicitation or offer to invest in a particular security or type of security. ZacksTrade does not endorse or adopt any particular investment strategy, any analyst opinion/rating/report or any approach to evaluating individual securities.
If you wish to go to ZacksTrade, click OK . If you do not, click Cancel.
Is Carnival (CCL) A "Buy" Heading into Q2 Earnings Announcement?
Cruise and vacation company Carnival ( CCL Quick Quote CCL - Free Report ) is set to report Q2 results on Tuesday before the opening bell. Carnival, a Zacks Rank #3 (Hold), has exceeded the earnings mark in each of the last six quarters. But amid recent signs of weakening summer travel demand, is Carnival a buy prior to the release?
Analysts are expecting the company to post a minor loss of -$0.01/share, reflecting a 96.8% improvement relative to the same quarter last year. Sales are projected to have increased 15.1% to $5.65 billion.
Carnival has surpassed earnings estimates in each of the past six quarters. The company has delivered a trailing four-quarter average earnings surprise of 22%.
Strong brand recognition and a strategic marketing campaign bode well for Carnival. The cruise liner remains focused on its fleet optimization and expansion. Still, travel demand has begun to normalize following the post-pandemic boom.
Our proprietary Zacks Earnings ESP predicts another earnings beat for the upcoming announcement. As always, investors should exercise caution ahead of any earnings release.
See More Zacks Research for These Tickers
Normally $25 each - click below to receive one report free:.
Carnival Corporation (CCL) - free report >>
Published in
This file is used for Yahoo remarketing pixel add
Due to inactivity, you will be signed out in approximately:

COMMENTS
Post-pandemic #anxiety is a real and common problem. But help is available to manage the rational and irrational stressors of re-entering society. Elspeth C. Ritchie, MD, MPH, discusses tips to reclaim your quality of life: https://bit.ly/2UlFyQ9. ... the U.S. is widely lifting domestic travel restrictions. Simultaneously, new virus variants ...
May 3, 2021 at 1:32 p.m. EDT. (Illustration by Whitney Wong for The Washington Post) For travelers with anxiety and panic disorders, vacations did not always feel like getaways, even before covid ...
Travel anxiety in a post-pandemic world. It turns out I'm not alone. Experts say travel anxiety rates are on the upswing—and while looming health, safety, and planning concerns are partly to blame, what we're experiencing goes beyond that. "'Re-entry anxiety' refers to the fear that can accompany letting go of the safeguards that ...
Some common causes of travel anxiety include: Fear of flying. One of the most common issues in people who have travel anxiety is the fear of flying. This fear might be triggered by: Air turbulence ...
Using trauma-informed tips to achieve safety, remembrance and reconnection will reduce re-entry anxiety. Here are a few to use: Make sure you communicate your needs to others as you begin your re ...
Dr Sarah Jarvis Post Covid Travel Anxiety. Author: Dr Sarah Jarvis, MBE, General Practitioner (GP) Dr Sarah Jarvis is the Clinical Director of the Patient Platform, an active medical writer, broadcaster, and the resident doctor for BBC Radio 2. 30th May 2022 8 min read. I think it's fair to say that for pretty much everyone, it has been a very ...
This anxiety is commonly experienced in the form of fear, nervousness, worry, or dread. What Underlies Re-Entry Anxiety? The level of uncertainty inherent in the COVID-19 pandemic has been anxiety-provoking for most people. Still, in recent months, many people had started to become habituated to a new way of life, one that was primarily spent ...
Post-Pandemic Anxiety: Feeling Stressed as Things Return to Normal. As COVID-19 vaccinations roll out across the U.S. and states begin lifting various restrictions, many have begun thinking and dreaming of life post-COVID. And while the thought of gathering with family and friends again, traveling and getting back to loved activities can feel ...
Plan what you can. Anxiety stems from feeling a loss of control, so the more people can exercise control, take control, and put controls in place, the calmer they will be, according to Greer. That means being very mindful, thoughtful, and intentional about the activities and plans you participate in post-pandemic.
Clinically speaking, hypervigilance is a trait of anxiety.So, in many ways, the pandemic may have taught some of us to be hypervigilant to stay safe. In military contexts, service members are ...
How to manage travel-related stress in the COVID era. It's perfectly normal to feel nervous about travel post-COVID—whether it's thinking you might get sick, or just because it's been a long time since you've done it. But focusing disproportionately on things we can't control causes anxiety and actually isn't going to do you any ...
April 14, 2021 at 12:00 p.m. EDT. Will we still want to stay home when the pandemic is over? (iStock) Thomas Plante is grounded — by choice. "The pandemic made me realize that I really would ...
Don't skip the self-care activities. Just because you may think you're in a time crunch the week before a trip, build in time for exercise. Physical activity is a great way to manage stress. Pamper yourself. A haircut or a manicure may be an important part of your pre-travel preparation to help you de-stress.
Then respondents were also asked about their travel plan post-lockdown. The predominant mode of transport for commuting to primary and secondary activities was asked and in addition to the trip length of primary activities. ... Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: the case of the 2009 H1N1 pandemic. Br. J ...
The localized and regionalized travel trends due to nationalistic thoughts, distrust, anxiety, and even hostility have intensified during the pandemic (Brouder et al., 2020) and may have a long-term adverse effect on post-pandemic travel and tourism.
After more than a year of social distancing and without knowing who is fully vaccinated, returning to 'normal' may feel scary, especially if you already live with anxiety, according to Dr. Susan Evans, Professor of Psychology in Clinical Psychiatry. "Anxious individuals worry," Dr. Evans says. "Whenever there is uncertainty about the ...
The COVID-19 pandemic has created an unprecedented and devastating impact on the travel and tourism industry worldwide. To sustain tourism organizations in the post-pandemic period, it is crucial to understand the factors that maintain, boost, or diminish the potential demands of international travel.
Partial correlation network analysis suggests that the chronic post-COVID neuropsychiatric symptoms can be clustered into two major (cognitive complaints -fatigue and anxiety-depression) and one ...
As a post-pandemic travel landscape awaits us, all we can do is build resilience. I hope this has been useful, this has been my experience with a really good group of adaptogens which have earned a place in my travel wellness toolkit. ... Travel Anxiety. Adaptogens. Supplements. Supplement Science. Self Help----Follow. Written by Christopher ...
Gateway — a nonprofit cinema located at 1550 N. High St. — reopened on May 27, 2021, after closing for the COVID-19 pandemic in March 2020.
In, "Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19A Meta-analysis," Nicole Racine et al. give an incredibly insightful analysis of the global increase in anxiety and depression in children and adolescents since the start of the COVID-19 pandemic[1]. This rise in anxiety and depression is ...
There's no end in sight to the high airfares that are a mainstay of the world's post-pandemic travel boom, according to Asia's biggest low-cost carrier. Travelers may see a little reprieve ...
According to the Advantage Travel Partnership's latest Global Business Travel Review, 2023 booking volumes reached 92% of 2019 levels, with 2024 expected to exceed pre-pandemic transactions by at ...
The global aviation industry has been transformed as the post-pandemic reopening unleashed a wave of pent-up travel demand that's sent ticket prices surging faster than inflation in many parts ...
(Bloomberg) — There's no end in sight to the high airfares that are a mainstay of the world's post-pandemic travel boom, according to Asia's biggest low-cost carrier. Travellers may see a little reprieve next year as jet fuel prices decline and the airline's flight capacity rises, said AirAsia Aviation Chief Executive Officer Bo ...
Traffic in Dallas has increased 12% compared to before the pandemic, according to the company's 2023 Global Traffic Scorecard. The report ranked Dallas as the 17th most congested city in the ...
Elektrostal is linked by Elektrichka suburban electric trains to Moscow's Kursky Rail Terminal with a travel time of 1 hour and 20 minutes. Long distance buses link Elektrostal to Noginsk, Moscow and other nearby towns. Local public transport includes buses. Sports
Analysts are expecting the company to post a minor loss of -$0.01/share, reflecting a 96.8% improvement relative to the same quarter last year. Sales are projected to have increased 15.1% to $5.65 ...
GENERAL AFFIDAVIT Russian Federation..... ) Moscow Oblast ..... ) City of Moscow.....
Yandex Maps will help you find your destination even if you don't have the exact address — get a route for taking public transport, driving, or walking.