Optimizing RVU Production In An Academic Medicine Practice
- Post author By James Allen, MD
- Post date June 8, 2019

The work RVU is the current medium of exchange in clinical practice for all physicians, both private and academic. And as the numbers of physicians employed by academic medical centers swells at the same time as the percentage of these physicians’ time dedicated to clinical practice grows, academic physicians in particular are under increasing pressure to maximize their RVU output. Consequently, many academic physicians find themselves struggling to produce their required numbers of RVUs. Historically, private practices were built around efficient RVU productivity but academic practices were not and consequently, the academic inpatient and outpatient practice environment and practice culture is not conducive to RVU maximization . Failure to meet annual RVU targets can result in loss of bonuses, salary reduction, career disillusionment, and general unhappiness. On the other hand, consistently meeting or exceeding RVU targets can provide job security and the freedom to chart one’s own career path in academic medicine. Here are some of the ways that academic physicians can optimize their RVU production.


In The Inpatient Setting:
- Don’t forget to submit your bill for your clinical services. This seems so simple but a few years ago, I did an analysis at our own hospital and found that 7% of inpatient services and procedures that were documented in the electronic medical record went unbilled. This was not because of a conspiracy by the physicians, it was simply because they forgot to enter a charge for a given day’s clinical work. It is easy to forget to submit a bill (often called the “charge capture” application in an electronic medical record). If you are busy trying to save a patient’s life, the lowest priority in your day is to put in a bill for that service. I consider myself pretty compulsive when it comes to billing and even I found times when I forgot to enter a bill for a consult, a return hospital visit, or a bedside procedure. Two strategies can help minimize forgotten charges: (1) work with your electronic medical record to create charge entry prompts when completing progress notes or procedure notes to make entering those charges easier and (2) develop a personal strategy to ensure that all services are billed each day – I print out a rounding list of all of my patients each day and note my E/M service & procedure charge on each patient as I enter charges; at the end of the day, I can take a quick look at the printout to confirm that every patient had a charge entered.
- Don’t avoid submitting a bill for your service. A number of years ago, one of our very best clinical educators stopped signing resident inpatient notes and inpatient charges. The excuse was that there just wasn’t enough time in the work day and it got in the way of bedside teaching. No note meant no bill for service. No bill meant no income. No income meant no job.
- Don’t under bill. Most large academic medical practices do billing audits by billing compliance personnel. These audits are largely defensive, designed to prevent over billing. This is because large medical practices (and particularly academic practices) are subject to billing audits by Medicare or other insurance companies. The bias from compliance audits is that it is better to err on the side of under billing than over billing. Over billing jeopardizes the organization but under billing jeopardizes the individual physician by making him/her do more work than is necessary to meet annual wRVU targets.

- There should be no such thing as a curbside consult. The curbside consult is when an admitting physician (or more likely a resident) asks an “off-the-record” clinical question of a consultant. There is no entry into the medical record by the consultant and there is no bill generated. If a consultant’s expert opinion is sought, that consultant should be paid for it. I was once an expert witness in defense of a university medical center. One of the residents had called a pathologist to ask an opinion about an inpatient case and made the mistake of documenting that conversation (and the pathologist’s name) in the medical record. The pathologist was named as a co-defendant in the malpractice suit. Even an off the record opinion can result in legal liability so you should bill for your expertise and opinion.
- Don’t sign-off too quickly. For many consulting physicians in academic practice, a major goal of the workday is getting the consult census list shortened as much as possible. Consult follow-up visits are beneficial to patient and the primary service because the consultant’s expertise can be applied to new test results and changes in the patient’s condition. This can reduce inpatient hospital length of stay. Those follow up inpatient encounters do not pay as much as initial consult encounters but they often take very little time and on a per-hour basis can generate more RVUs per hour than initial consults. Most initial inpatient consults require at least 2-3 follow-up visits and many will require daily follow-up visits until the patient is discharged. In academic practice, there is a strong tradition of being a “one and done” when it comes to consults. For a consultant, those follow-up visits take far less time than a follow-up visit by the admitting service (hospitalist, etc.) so you can perform a lot of follow-up visits in an hour. I believe that this is the #1 low-hanging fruit in academic medicine for increased wRVU generation .

- Mundane tasks generate a lot of wRVUs but can melt your brain. EKGs and pulmonary function tests are commonly performed in large medical centers. On an individual basis, neither generates very many work RVUs. However, they take very little time to interpret and document and consequently, the cardiologist or pulmonologist can generate huge numbers of wRVUs very quickly. The problem is that reading PFTs and EKGs is boring and are often seen as an unpleasant necessity of specialty practice. My brain would melt if the only thing I did all day was read PFTs but by reading them for an hour or two a week, I can generate enough wRVUs to free me up to do the uncompensated things that I really like to do.

- Make your EMR work for you. Investing a little time developing disease-specific note templates, order sets, and order preference lists can pay enormous long-term benefits by creating time-saving shortcuts in your electronic medical record charting. I have different new consult templates for the inpatient conditions that I most commonly encounter: COPD exacerbations, pneumonia, asthma exacerbations, abnormal chest x-ray, pulmonary embolism, etc. I incorporate my own self-designed “smart lists” into the physical exam portion of my notes that default to the expected findings; for example, for an asthma consult note, the lung exam smart list defaults to “diffuse wheezing” whereas the pulmonary embolism consult lung exam smart list defaults to “normal breath sounds bilaterally”. This allows me to rapidly click through the physical exam and saves me precious keystrokes when creating my consult note. Copying and pasting can also shorten your documentation time but it can be hazardous if you are copying too much data from a previous day’s progress note because of the danger of importing out-of-date information (like vital signs, lab results, NPO status, etc.). By using templates for notes that automatically import new data into the daily note, you can avoid this. I limit my copying/pasting to just my “impression and plan” list so that I can remember what problems I am actively following and what my previous day’s recommendations were – I then edit the impression and plan as appropriate.

- You will get more efficient producing RVUs with age. There is a Starling curve of physician productivity. It takes about 7 years after finishing residency or fellowship to get proficient in getting clinical work done. Not only do physicians continue to learn new knowledge but they get more efficient in getting their daily work done with everything from history taking to progress note writing. For most physicians, productivity peaks in their mid-50’s. After that, they often start dialing back the amount of time they spend in clinical practice.
In The Outpatient Setting:
- Pre-chart your patient encounters. Each outpatient encounter will require a certain amount of time in the patient exam room and a certain amount of time outside of the exam room. You can either finish your charting at the end of the day, after the patient leaves or you can do that additional charting before the patient arrives in the clinic. Either way, it will be the same amount of time – either before clinic or after clinic. But by pre-charting and preparing for the patient’s visit, you can often shorten the amount of time spent during actual clinic hours – this can free you up to spend more time communicating with individual patients and allow you to see more patients in a given period of time.
- Utilize CPT code 99358. This code is for “prolonged service without patient contact”. It requires documentation that you spent at least 31 minutes doing the service and I primarily use it (1) when reviewing a lot of medical records in advance of a new outpatient consult or (2) after an initial consult when I receive a lot of requested records and radiographic images. In my own practice, most new outpatients come with lots of chest x-ray & CT images that I need to review and interpret, office notes that I need to review, lab results I need to review, and pulmonary function tests that I need to review and interpret. About half of my new patients have > 31 minutes of records to be reviewed and documented. This CPT code is worth 2.10 wRVUs and when combined with a level 5 new outpatient visit (3.17 wRVUs), you can generate a whopping 5.27 wRVUs (7.91 total RVUs) for that visit. I use this code 2-3 times a week. Also, if that new patient does not show up, I still am able to generate some wRVUs for my efforts.
- Utilize the other CPT codes that you forgot to bill. The common ones are 99497 (advanced care planning, 30 minutes: 1.50 wRVUs), 99406 (smoking cessation 3-10 minutes: 0.24 wRVUs), 99495 (transition care management, moderate complexity: 2.11 wRVUs), and 99354 (prolonged services > 30 minutes: 2.33 wRVUs). I wrote about these and other often-overlooked CPT codes in a previous post .
- Cultivate a referral base. For specialists, new patients can come from self-referrals, emergency department referrals, or physician referrals. Self-referrals and ER referrals are notorious for being no-shows and for having no insurance (or having Medicaid). You are better off filling your schedule with referrals from primary care providers and other specialists because those patients are more likely to show up for their scheduled appointment and generally constitute a better payer mix. The best way to cultivate those referrals is by human contact, either introducing yourself in person or by the occasional phone call. Those referral physicians will remember your name the next time they need a consult if they have shaken your hand or heard your voice. This is especially true for nurse practitioner or physician assistant primary care practices – NPs and PAs don’t have the same opportunities to network with specialists at medical staff meetings, the hospital’s physician lounge, or CME events. A phone call to a primary care NP can endear you to him/her for life. Referral letters are also a good way to cultivate referrals. Each referral letter is an advertisement opportunity for your practice: a poorly constructed letter that consists of 4 pages of electronic medical record documentation will create animosity but a 1-paragraph readable note in prose form will create goodwill.
- Make the outpatient EMR work for you. Reducing keystrokes saves you time that you can spend seeing more patients and generating more wRVUs. Just as in the inpatient setting, by creating note templates for common conditions that you use, you can reduce your documentation time; in my pulmonary practice, I have different templates for COPD, interstitial lung disease, asthma, abnormal x-ray, and bronchiectasis office notes. Pre-designed order preferences and smart lists can streamline your practice. Outpatient EMR optimization is a huge topic and I’ll devote a post just to this in the future.

- Convert patient phone calls into wRVUs. There are two ways to do this: get the patient into the office or use the new CPT code for telephone/EMR encounters. CPT code G2012 is for phone or EMR patient encounters that last 5-10 minutes for patients that are not seen for 7 days before or 24 hours after the phone/EMR encounter. It pays 0.25 wRVUs. The other strategy is to get those patients into the office – either at the end of the day or to fill in holes in the office schedule created by late cancelations. Alternatively, keep a open 15 or 30 minutes at the end of the day for add-on sick visits. I prescribe way too much steroids/antibiotics over the phone for COPD exacerbations, etc. that could at least be billed as a G2012.

- Use the entire day. I often see physicians start their morning schedule at 9:00 even though the nurses and registration staff all arrive at 7:30. Similarly, I see physicians schedule their last patient at 3:30 or 4:00 even though the staff are paid to be there until 5:30. Time = wRVUs. Be sure to fill the entire day’s clinic time with patients.
- Double book strategically. In my practice, there are almost always late cancelations and no-shows. By double booking a couple of slots in expectation of those cancelations and no-shows, you can ensure that the schedule stays full. I often see physicians double book at the beginning of their schedule – I think this is hazardous because if both patients show up, then the physician is behind the schedule for hours, creating exasperation for the physician and dissatisfaction for the patients. I think you are better off double booking a slot in the middle of the morning (or afternoon) and at the end of the day. this is because there are inevitably patients who show up 30 or 45 minutes early for their appointments so if there is a late cancelation, you can slip an early arriver into that slot, thus creating an opening in the middle of the afternoon (or morning) or at the end of the day that the double booked patient can fill.
- Make up canceled clinics. There should not be an expectation for making up clinics canceled for vacations and scheduled CME time off. However, in academic practice, there are always things that come up that conflict with the regular clinic times: academic retreats, medical staff meetings, visiting lecturers, new faculty candidate interviews, medical student lectures, etc. These activities fall under “academic time” (release time) and when those conflict with regular clinic time, necessitating canceling that afternoon’s clinic, then a make-up clinic should be scheduled. If your academic time temporarily displaces your usual clinic time then you should have an equal displacement of your usual academic time by make-up clinic time in order to keep your total weekly academic:clinic time ratio constant.
- Do point of care testing. For me, this means having an office spirometer (0.17 wRVUs per test). For others, it may mean an INR machine, an EKG machine, or a hemoglobin A1C machine. In order to determine if you need a piece of equipment to do point of care outpatient testing, you have to do a pro forma that compares the cost of the equipment to the estimated income generated by that piece of equipment. It takes about 44 spirometry tests to pay for the cost of a spirometer, after that, all of the income generated by spirometry is profit.
- Partner with advanced practice providers. Everyone wants an NP/PA/LISW/pharmacist in order to make their practice more efficient and generate more wRVUs. But everyone also wants someone else to pay for that NP/PA/LISW/pharmacist. In a healthy clinical environment, the physician should work synergistically with advanced practice providers so that the total RVU productivity is greater than the sum of what that physician & advanced practice provider could generate operating individually. Examples are a physician assistant who does the post-op office visits so that the surgeon can do more surgeries or a nurse practitioner who sees routine follow-up heart failure visits so that the cardiologist can see more new patient consults that in turn lead to more cardiac stress tests and echos.
June 8, 2019
By James Allen, MD
I am a Professor Emeritus of Internal Medicine at the Ohio State University and former Medical Director of Ohio State University East Hospital
Blog / 2023 Physician Work RVU Increases Finalized by Medicare
The 2023 Medicare Physician Fee Schedule Final Rule was released on November 1, 2022. The final rule includes CPT code changes recommended by the American Medical Association (AMA). The changes are numerous and vary in type, but the result is an overall increase in work Relative Value Units (RVUs) for nearly all physicians who provide evaluation and management (E&M) services in hospitals and nursing facilities .
Key Takeaways
- The 2023 Medicare Physician Fee Schedule Final Rule adjusts CPT codes as per AMA recommendations, raising work RVUs for most hospital and nursing facility-based physicians.
- Significant updates to work RVU values for specific E&M services include notable increases for commonly used billing codes.
- Code restructuring merges several hospital observation and home visit service codes, affecting billing practices across specialties.
- Changes impact various specialties differently, urging facility-based specialists like hospitalists and geriatricians to update billing strategies.
2023 Inpatient E&M Code Changes
The Medicare Physician Fee Schedule Final Rule (2023 Final Rule) includes both increases and decreases in work RVU values for E&M services provided in hospital and nursing facility settings. Generally, the most used billing codes (99232, 99233, 99308, and 99309) within this subset are all going to realize double digit increases in work RVUs.
Table 1: Proposed 2023 E&M Code Updates
Source: Comparison of 2023 Final Rule to RVU22C
The work RVU changes in the 2023 Final Rule are more complex than those in the 2021 Final Rule. The 2021 Final Rule only increased work RVUs for seven outpatient services codes. Forecasting the 2023 Final Rule accurately requires crosswalking many deleted codes with substitute codes. The AMA and Medicare have deleted hospital observation E&M procedure codes and merged those services into the codes for hospital inpatient E&M services. Visit codes for E&M services in assisted living and custodial care facilities are also being consolidated into the general home visit service codes.
Table 2: 2023 Deleted Codes & Substitutes
Source: AMA CPT Evaluation and Management Code and Guideline Changes
2023 Overall Medicare Work RVU Impact by Specialty
LBMC calculated the overall work RVU impact of the 2023 Final Rule changes by specialty by applying the new work RVU values to the billing data contained in the public 2019 Medicare Provider Utilization and Payment data set.
This analysis indicates that hospitalists, infectious disease physicians, geriatricians, PM&R, hematologists, psychiatrists, internists, palliative care, and other specialists who practice in hospital and nursing facilities will realize the most increases in work RVUs from the 2023 Final Rule changes. Advanced Practice Providers (APPs) specializing in geriatrics, acute medicine, mental health, and other facility-based specialties are similarly affected.
When combined with the 2021 outpatient E&M changes, dozens of specialties will realize double-digit increases in work RVUs.
Table 3: Estimated Overall Changes in Work RVUs by Specialty
Note: Overall wRVU % change by specialty does not reflect the skewed impact within specialties. Disclaimer: No estimate is made for changes in existing coding patterns other than substitutes.
Highly Variable Work RVU Impacts within Specialties
The overall work RVU increases projected in the previous section do not reflect the expected variation in work RVU changes among physicians within each specialty. The 2023 Final Rule includes both increases and decreases in work RVUs among the CPT codes affected. The severity and complexity of patient illnesses varies from physician-to-physician within each specialty. The proportion of E&M services provided in hospitals, offices, and nursing facilities can also vary substantially within specialties like hospital medicine, psychiatry , and geriatrics .
For example, the table below summarizes the separate and combined changes for the 2021 Final Rule and 2023 Final Rule. The percentage changes from 2020 to 2021 in the left-most column illustrate the distribution of work RVU increases exclusively for outpatient E&M services. The percentage changes from 2022 to 2023 in the center column illustrate the distribution of work RVU increases exclusively for inpatient E&M services. The percentage changes in the right-most column illustrate the combined effects of both the 2021 and 2023 rules. Predictably, the sample of 13,529 hospitalists analyzed in the following table were not impacted by the 2021 outpatient E&M work RVU changes at all. The variation of inpatient E&M service severity and coding among these hospitalists yields a wide range of estimated effects from 2% decreases in work RVUs at the 10 th percentile to 15% increases in work RVUs at the 90 th percentile.
Table 4: Estimated Work RVU Change Variability within Hospital Medicine (n=13,529)
Disclaimer: No estimate is made for changes in existing coding patterns other than substitutes
Forecasts estimate about half of physicians practicing Geriatric Medicine will realize increases in work RVUs during 2023 as a result of E&M updates for both inpatient and nursing facility services. When combined with the prior outpatient E&M changes from 2021, nearly all geriatricians are forecast to experience work RVU increases from 2020 to 2023.
Table 5: Estimated Work RVU Change Variability within Geriatric Medicine (n=3,013)
Adapting to changes in work rvu production, compensation & reimbursement.
On a combined basis, the 2023 Final Rule and the 2021 Final Rule materially change the Resource-Based Relative Value System on which physician reimbursement, productivity, and compensation is built. Commercial insurance carriers will not emulate Medicare’s changes in their own reimbursement systems overnight. Accordingly, an added level of thoughtfulness is required when using industry compensation and production surveys to set physician compensation. Employers of specialists that were unaffected by the 2021 Final Rule may find that they are materially affected by the 2023 Final Rule.
The path forward begins with identifying the financial impact of the 2021 and 2023 work RVU changes on production, compensation, and reimbursement for your healthcare professionals. Once the financial impact is known, the various options of partially or fully adopting the new production system changes can be assessed within your budgetary resources and restrictions.
LBMC Advisory Services has a team of experts exclusively dedicated to physician compensation analysis, planning, strategy and valuation. Contact LBMC today for assistance with productivity and compensation forecasts, scenario analyses, compensation planning, and questions regarding the impact of the 2023 Final Rule on Fair Market Value compensation analysis.
LBMC’s Nick Newsad recently discussed how the 2023 Medicare Physician Fee Schedule Rule will affect physician productivity measurement, compensation, and reimbursement during a webinar on August 4, 2022. Watch the webinar On-Demand: https://www.lbmc.com/blog/webinar-new-physician-work-rvu-increases/
Nicholas A. Newsad, MHSA works in the Advisory Services Group at LBMC. He can be contacted at [email protected] or 615-309-2489.
We’re happy to answer any questions you may have on what our experts can do for you. Please send us an email using the form and one of our professionals will get back to you promptly.
Privacy Overview

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
ACC 2023 Physician Fee Schedule Calculator Now Available
Acc news story.
The Center for Medicare and Medicaid Services (CMS) posted a revised file on Jan. 5, 2023 that rendered several RVU inputs and the conversion factor outdated due to changes required by recent year-end spending legislation. Revisions to the calculator file are complete and the version now posted here reflects those updates.
Work, practice expense and liability relative value units (RVUs) are updated annually through Medicare Physician Fee Schedule rulemaking. In response to the recently finalized 2023 Medicare Physician Fee Schedule and related addenda , the ACC developed a new Physician Fee Schedule Calculator . This tool allows clinicians and practice managers to estimate the impacts of the slated changes to practices. Over time, the goal of the tool is to help facilitate a thorough understanding of impacts from one year to the next. Download the tool.
Want a more in-depth look at 2023 Physician Fee Schedule changes? Stay tuned to ACC.org and MedAxiom in the coming weeks.
Keywords: Medicare, Fee Schedules, Physicians, Relative Value Scales, ACC Advocacy
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Contact Member Care
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
I'm looking for
- Foundation for Women’s Cancer
- Risk Factors
- First Appointment
- Diagnostic Tests
- Treatment Options
- Post Treatment
- Lynch Syndrome
- Clinical Trials
- Survivorship Toolkit
- Search Site
Telemedicine Coding Examples
Josh Cohen, MD; Mark Shahin, MD; David Holtz, MD; Susan Zweizig, MD
Download PDF
In follow up to the SGO April 10, 2020, webinar entitled “Telemedicine for Gynecologic Oncology Care During the COVID-19 Pandemic,” below are a series of eight clinical scenarios for telemedicine coding. On March 17, 2020, the Centers for Medicare and Medicaid Services (CMS) agreed to pay providers to care for Medicare beneficiaries for office and hospital visits via telehealth anywhere in the United States. This went to effect retroactively on March 6, 2020, and will continue through the COVID-19 pandemic. Each clinical case has an example of how to code the encounter. This will vary on geographic location, practice setup, and changing regulations with COVID-19. After the clinical case scenarios there is a list of resources to assist with coding.
Clinical Scenario 1
A 54-year-old woman with prior history of stage IVB endometrial cancer. She was diagnosed in 2018. Most recently she has been on a combination of letrozole and everolimus for 6 months. She had a CT recently and has an upcoming visit. She was encouraged to have a telehealth visit as she was not enthusiastic about leaving her house and traveling to our office during the pandemic.
The office staff contacted her and instructed her on how to set up a telehealth visit on the platform for our enterprise. Ten minutes before the visit she contacted the office to say that she was having difficulty signing on. Despite multiple attempts, she could not establish a video connection, and the visit was conducted by audio on phone only. Typically, our audiovisual platform allows for consent of the patient when signing on, but this could not happen. Upon establishing audio connection, the provider reviewed with the patient the exact same consent process, identified her and the patient understood that she will receive a charge for services performed. She agreed to this.
Her current symptoms were reviewed, and an interim history was obtained from the past 4 weeks, as she had been seen by the office NP at that time. Since her last visit she is having a great deal of joint pain—some related to letrozole, but also due to recurrence in the pelvis resulting in a fracture of left pubic bone and enlargement of the tumor in adductor muscles. She is experiencing anemia from everolimus. She has proteinuria and is managed by nephrology, and her Cr level remains stable. Her most recent CT shows progression of disease with development of malignant ascites and pleural effusion.
During this visit the provider and patient did the following:
- Reviewed a new treatment plan with pembrolizumab and lenvatinib, including all side effects and expected response rates, frequency of treatments, and imaging for assessment of response was determined.
- Discussed several modalities of pain management, including availability of medical marijuana and risks, benefits.
- Discussed her ongoing but relatively stable medical issues including diabetes, nephropathy and hypertension and the effects of this treatment on them. Dosing of lenvatinib was reduced for reasons related to her hypertension.
- Discussed issues related to her goals of treatment, availability of social support at home, ability to accomplish her goals and finally reconsidered her living will and durable Power of Attorney (POA).
Diagnoses: C54.1 Endometrial cancer, C79.51 Metastasis to bone, R18.0 Ascites, J90.0 Pleural effusion, M25.351 Pain, right hip, M54.9 Back Pain, E11.9 Diabetes, R80.9 Albuminuria
Time spent face-to-face today was 25 minutes with an additional 10 minutes used to document. Medical decision making was high and complex. In the documentation of the encounter, the failed attempt at telehealth was noted as was the patient’s verbal consent for the encounter. Total minutes for the encounter was documented in the note.
99214-GT (2.22 RVU) Level 4 was selected based on complexity of medical decision making even though an exam was not performed. Some would argue a Level 5 (99215-GT, 3.14 RVU) charge may even be appropriate here given the complexity, but it really depends upon the time you have documented in the chart and complexity you have portrayed. Time of the visit was considered. GT modifier was added for telehealth platform. Modifiers are a way to communicate to the payer that the charge is being submitted under special circumstances. The -95 modifier is appropriate for Medicare patients who have telehealth visits. And –GT is also a modifier for non-Medicare patients indicative of a Telehealth visit.
Clinical Scenario 2
A 71-year-old woman with a history of Stage IB, grade 3 endometrial cancer 4 years ago due for her routine surveillance visit during the COVID-19 pandemic crisis. She lives in New Jersey, and the physician practices in Pennsylvania.
The office staff has called the patient to change her office visit to a telemedicine visit after confirming her access to a computer and that she has no specific concerns.
After establishing a video conference line with her and exchanging pleasantries, the physician obtained consent with the following script that is in the note:
“Hello, my name is Dr. (Insert Name). Before we proceed, can you please verify your identification by telling me your full name and date of birth? Can you tell me who is in the room with you?
“You and I are about to have a telemedicine check-in or visit because you have requested it. This is a live video-conference. I am a real person, speaking to you in real time. There is no one else with me on the video-conference. However, when we use (FaceTime, Skype, etc.) it is important for you to know that the video-conference may not be secure or private. I am not recording this conversation and I am asking you not to record it. This telemedicine visit will be billed to your health insurance or you, if you are self-insured. You understand you will be responsible for any copayments or coinsurances that apply to your telemedicine visit. Before starting our telemedicine visit, I am required to get your consent for this virtual check-in or visit by telemedicine. Do you consent?”
Patient Response to Request for Consent: “Yes”
The provider reviewed and documents that there are no changes to her medical, surgical, social or family histories, her medications and allergies. The provider documents a review of systems, and goes over her blood pressures from the patient’s home BP cuff, which are sometimes 140/80. The provider assures the patient she has no symptoms consistent with recurrent endometrial cancer.
They review symptoms of endometrial cancer, discuss the importance of taking her BP meds daily but to call her medical doctor or gynecologic oncologist if the BPs continue to stay elevated. The provider sends a screening mammogram script to her, and they plan for a full examination in 6 months. The physician documents that 26 minutes were spent on the call.
Diagnosis: C54.1 Endometrial cancer, I10 Hypertension Final Code: 99214-95 (2.22 RVU)
Office encounters like this are a daily fact of life during the current pandemic, and may continue to be performed in the foreseeable future. This case demonstrates two things: E&M coding can be done with video telemedicine visits and interstate telemedicine is allowable under certain circumstances.
CMS has recently published a good summary statement about telemedicine during the pandemic crisis: cms.gov/files/document/covid-19-physicians-and-practitioners.pdf . For this case, the key points are a documented complete update to the history and the level of Medical Decision Making. A provider can bill for a Level 4 visit since because one chronic stable problem (endometrial cancer) and a chronic worsening issue (hypertension) are being addressed. Documenting the time taken to perform the video chat, as well as any preparation or documentation, can also establish a level of service.
Second, CMS is allowing interstate telemedicine care if it is allowed by the state medical licensing rules. In this case, New Jersey is temporarily letting out-of-state physicians practice with only an online application. Pennsylvania requires a written request. You should check with the state authorities in your state as well as your patient’s state to see your local requirements. For the duration of the COVID-19 emergency, CMS is permitting interstate telemedicine.
Last, for any E&M coding for telemedicine, the -95 modifier is added to indicate a video telemedicine encounter.
Clinical Scenario 3
A 78-year-old with new diagnosis of grade 2 endometrial cancer on EMB presents for telemedicine encounter. She is called by the office medical assistant 10 minutes before her visit and instructed on how to sign into the patient portal application through her smartphone. Upon logging in for the visit she reads the following statement and agrees in order for the telemedicine encounter to begin.
Name of patient – I agree to be treated via a video visit and acknowledge that I may be liable for any relevant copays or coinsurance depending on my insurance plan. I understand that this video visit is offered for my convenience and I am able to cancel and reschedule for an in-person appointment if I desire. I also acknowledge that sensitive medical information may be discussed during this video visit appointment and that it is my responsibility to locate myself in a location that ensures privacy to my own level of comfort. I also acknowledge that I should not be participating in a video visit in a way that could cause danger to myself or to those around me (such as driving or walking). If my provider is concerned about my safety, I understand that they have the right to terminate the visit.
- Reviewed endometrial cancer treatment options including surgery, empiric radiation, and hormonal management.
- Discussed risks, benefits, alternatives to surgery.
- Planned for preoperative medical clearance with referrals, orders for imaging and laboratory tests were placed.
- Discussed postoperative recovery expectations and follow up.
- Reviewed adjuvant treatment scenarios after surgery.
Time spent face-to-face was 45 minutes and an additional 15 minutes was used to document. Medical decision making was high and complex. A statement including the patient’s consent was included in the encounter. Total minutes for the encounter was added to the note.
Diagnosis: C54.1 Endometrial cancer, N95.0 Postmenopausal bleeding, Z71.9 counseling non specified
Final Code: 99204-95 (RVU=3.67), considering adding modifier GT. GT modifier can be added for telehealth platform visits. Modifiers are a way to communicate to the payer that the charge is being submitted under special circumstances. A -95 modifier is appropriate for Medicare patients who have telehealth visits. The –GT is also a modifier for non-Medicare patients indicative of a telehealth visit.
Prior to the pandemic, telehealth visits were not allowed for new patients and only used for established patients. Due to recent guidelines by CMS, new patient visits are allowed to bill for telehealth services.
Clinical Scenario 4
A 52-year-old BRCA2 mutation carrier established patient with stage IIIC ovarian cancer on maintenance PARP after upfront chemotherapy presents for a telemedicine encounter. She is called by the office medical assistant 10 minutes before her visit and instructed on how to sign into the patient portal application through her smartphone. The visit pertains to toxicity of the PARP with fatigue and nausea with discussion of surveillance plan and labs.
- Reviewed PARP dosing with possible dose reduction if symptoms do not improve.
- Reviewed management of nausea and fatigue with prescription for Zofran and Reglan sent to pharmacy and TSH ordered.
- Reviewed Lab frequency with new labs ordered monthly for PARP and CA-125 ordered every 3 months.
- Reviewed signs and symptoms of recurrence and potential indications for CT imaging
- Reviewed issues related to her goals of treatment, availability of social support at home, ability to accomplish her goals and finally reconsidered her living will, and durable POA.
Time spent face-to-face today was 20 minutes and an additional 10 minutes was used to document. Medical decision making was high and complex. A statement including the patient’s consent was included in the encounter. Total minutes for the encounter and documentation after the visit was added to the note.
Diagnosis: C56.1 Ovary Ca, right, C56.2 Ovary Ca, left, Z15.02 BRCA mutation, R53.83 fatigue, unspecified, R11.0 Nausea
Final Code: 99214-GT (RVU= 2.22), considering adding modifier GT. Modifiers are a way to communicate to the payer that the charge is being submitted under special circumstances. The –GT is a modifier for non-Medicare patients indicative of a telehealth visit.
Clinical Scenario 5
An 85-year-old with newly discovered 6 cm adnexal mass presents for telemedicine encounter. Telemedicine fails. She is called by the office medical assistant 10 minutes before her visit and instructed on how to sign into the patient portal application through her smartphone. The patient is unable to login with her smartphone or computer technology for an audiovisual encounter. The provider calls the patient instead on the phone. Upon establishing audio connection, the provider reviewed with the patient the exact same consent process, identified her and she understood she will receive a charge for services performed. She agreed to this.
- Discussed the complete history with a 14-point review of systems.
- Discussed imaging and prior laboratory tests.
- Reviewed differential diagnosis and management options.
- Discussed surgical approach, risks, benefits, alternatives and recovery.
- Obtained verbal consent for surgery.
Time spent face-to-face today was 35 minutes and an additional 15 minutes was used to document. Medical decision making was high and complex. A statement including the patient’s consent was included in the encounter. In the documentation of the encounter, the failed attempt at telehealth was noted as was the patient’s verbal consent for the encounter. Total minutes for the encounter was documented in the note.
Diagnosis: R19.03 Pelvic mass, right, Z03.89 Observation for suspected malignancy and any other pertinent comorbidities Final Code: 99204-95 (RVU=3.67). Modifiers are a way to communicate to the payer that the charge is being submitted under special circumstances. A -95 modifier is appropriate for Medicare patients who have telehealth visits. At this time, CMS will allow for failed telehealth encounters to be billed as telemedicine encounter with specific documentation (attempt for audiovisual connection, verbal consent, and total time for the encounter). This is institutional/practice dependent as well and may change with the landscape of the current pandemic.
Clinical Scenario 6
A 64-year-old with stage IIIC ovarian cancer has postoperative pain and redness near incision 14 days out from surgery. The patient lives two hours away. She presents for a telemedicine visit. With visual technology no drainage or dehiscence is seen. Bactrim is ordered for presumptive wound cellulitis. Precautions upon when to go to the ER or seek medical attention are given. There were15 minutes spent face-to-face and 5 minutes on documentation.
- Reviewed signs and symptoms of infection, likely wound cellulitis.
- Discussed pathology and treatment recommendations for chemotherapy.
- Discussed wound care and starting oral antibiotics.
- Bactrim sent to pharmacy for patient to start today.
Time spent face—ace today was 20 minutes and an additional 10 minutes was used to document. A statement including the patient’s consent was included in the encounter. Total minutes for the encounter was added to the note.
Diagnosis: Cellulitis L03.311, Ovary Ca Right C56.1, Ovary Ca Left C56.2
Final Code: 99024-GT (RVU=2.22). Code 99024 is used because this is a postoperative visit that falls within the 90-day global coverage for surgery. A separate bill collection is not recommended as this does not represent a new process or issue that requires counseling unrelated to the patient’s surgery. Modifiers are a way to communicate to the payer that the charge is being submitted under special circumstances. The –GT is a modifier for non-Medicare patients indicative of a telehealth visit.
Clinical Scenario 7
A 70-year-old established patient sends an inquiry through digital portal discussing her symptoms while on olaparib maintenance therapy. She has recurrent ovary cancer, and has completed 6 cycles of chemotherapy with gemcitabine and carboplatin now almost 12 weeks ago with a partial response. She has been on olaparib for 6 weeks. She was seen 2 weeks ago, and a dose reduction was performed, now to 250 mg orally BID. Dose reduction was in response to severe nausea and anorexia. She reports her symptoms have improved although not fully resolved. She also is reporting fatigue.
In response to her the physician reassures patient and advises continued use of Zofran daily. Option of continued use of medical marijuana was reviewed. Finally, option of use of low dose methylphenidate at 5 mg for fatigue was offered.
In a communication back from the patient, she asks for new prescription for Zofran to be sent to her pharmacy. She wants to try the current dose for additional 2 weeks and will be evaluated in office at that time. In total review of the e-messages, responses, and writing the new prescription took 15 minutes.
Diagnosis: Cáncer of right ovary C56.1, Nausea R11.0, Fatigue R53.83
Final Code: 99422-95 (RVU= 0.72), considering adding modifier GT. The GT modifier can be added for telehealth platform visits. Modifiers are a way to communicate to the payer that the charge is being submitted under special circumstances. The -95 modifier is appropriate for Medicare patients who have telehealth visits. The –GT is also a modifier for non-Medicare patients indicative of a telehealth visit.
E-VISITS: In all types of locations, including the patient’s home, and in all areas (not just rural) established Medicare patients may have non-face-to-face patient-initiated communications with their doctors without going to the doctor’s office by using online patient portals. These services can only be reported when the billing practice has an established relationship with the patient. For these E-visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. The patient must verbally consent to receive virtual check-in services. The Medicare coinsurance and deductible would apply to these services.
Medicare Part B also pays for E-visits or patient-initiated online evaluation and management conducted via a patient portal. Practitioners who may independently bill Medicare for evaluation and management visits (for instance, physicians and nurse practitioners) can bill the following codes:
- 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes
- 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11– 20 minutes
- 99423: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes.
Clinical Scenario 8
66-year-old female with newly diagnosed stage IVB papillary serous uterine cancer and COVID-19 infection admitted for shortness of breath and bilateral pleural effusions. She was admitted to the ICU and bilateral chest tubes were placed. The initial plan was for palliative chemotherapy once she was medically stable, however, the patient developed rapid disease progression while in the hospital and on hospital day 11 her goals of care were changed to comfort measures only. She had several impediments to discharge to inpatient hospice including the fact that she remained intermittently COVID-19 positive for 48 days. The patient was transferred to the gynecologic oncology service for management of her end-of-life symptoms where she remained for 15 days until she was cleared from COVID-19 infection and could be transferred to a hospice program. Total length of hospitalization 26 days.
During this hospitalization, gynecologic oncology:
- Provided initial consultation to the ICU team.
- Discussed initial plans for treatment with the patient.
- Broke the news about disease progression to the patient in the virtual presence of her family who was off site during the pandemic.
- Were responsible for 24-hour inpatient coverage, all orders and daily rounding.
- Held multiple prolonged goals of care discussions with the patient and her family along with palliative care.
Time spent face-to-face via audiovisual communication was 35 minutes on day 1 and an additional 15 minutes was used to document. Medical decision making was high and complex. A statement including the patient’s consent was included in the encounter. Total minutes for the encounter was documented in the note daily.
With the gynecologic oncologist in the same building but not in direct contact with the patient, this visit, even though performed via remote audiovisual technology, would still be coded the same as if the attending were in the room with the patient.
- Place of service 21 is the modifier to denote this encounter took place in the inpatient setting with the provider in the same building. This 2-digit code defines where the service occurs. The case scenario above would still be an inpatient service and not considered telehealth since provider and patient are located in the same building despite use of audiovisual technology
- POS 02-Place of service for telehealth: This would be the 2-digit code used for services provided by a physician located in a different setting (different building) other than the patient in the hospital via audiovisual technology (e.g. Zoom, Microsoft Teams, Doximity, etc.)
- If there is no resident/fellow, but rather a video screen that a nurse puts in the room for the attending to perform an audiovisual consultation visit with an inpatient, the billing is the same as above. The provider must ensure for the evaluation and management documented is consistent with what is normally reflected in the CPT codes billed. For example, if billing by components, the provider must ensure the level of billing meets the specifics for that level regarding history, physical exam, and medical decision making or meeting the time requirements if billing based on time regarding total face-to-face time in discussion and what was discussed.
When there is one provider rounding for the primary team, video visits may only be used for subsequent patient (“follow-up”) visits and not for initial patient assessments/consults. Consultants/consultation teams may employ video rounding for both initial and subsequent patient visits, under the following circumstances:
- If it is clinically determined that components of a physical exam can be performed via video or that no physical exam is medically necessary for the patient.
- If the video visit is not for urgent medical conditions (e.g. chest pain, shortness of breath).
- If the logistics of the consultation can be managed in a manner acceptable to the primary team, nursing unit, and the consultant.
- House staff performing an inpatient video visit must be supervised by an attending physician. Supervising physicians will direct the care of the patient and provide the appropriate level of supervision based on the complexity of care and the experience, judgment and level of training of the house staff being supervised. The supervising attending may select and employ the modality of supervision (Zoom, Microsoft Teams, etc.)
At all times, it is the responsibility of the physician seeking to perform the video visit to determine, within his/her clinical judgment and prior experience, whether an adequate exam can be achieved via video with that patient at that time. If the conclusion is that an adequate exam cannot be achieved, it is the obligation of that physician to make alternative arrangements that address the clinical circumstance including the following:
- Seeing the patient face-to-face.
- Making another effort to perform an audiovisual visit at a later time.
- Reviewing the chart and discussing the case with the primary team, to evaluate whether the consultant recommendations can be safely and adequately provided in the absence of an in person or video visit.
Depending on type of service the physician is providing, the codes remain the same regardless of in person or telehealth: Initial hospital consultation for non-Medicare patients: 99251-99255, Initial hospital care 99221-99223, Subsequent Hospital Care 99231-99233
Diagnosis: C54.1 Endometrial cancer, U07.1 COVID-19 virus identified
Final Code: Day 1 99222 (place of service-21) (RVU=3.87) , subsequent days 99231(place of service -21) (RVU= 1.11). Place of service 21 is the modifier to denote this encounter took place in the inpatient setting with the provider in the same building. This 2-digit code defines where the service is rendered. The case scenario above would still be an inpatient service and not considered telehealth since provider and patient are located in the same building despite use of audiovisual technology. POS 02-Place of service for telehealth:
This would be the 2-digit code used for services provided by a physician located in a different setting (different building) other than the patient in the hospital via audiovisual technology (e.g. Zoom, Microsoft Teams, Doximity, etc.)
RVU values (this may vary depending on your institution and use of modifiers)
RVUs are the basic component of the Resource-Based Relative Value Scale (RBRVS), which is a methodology used by the Centers for Medicare & Medicaid Services (CMS) and private payers to determine physician payment. RVUs define the value of a service or procedure relative to all services and procedures. RVUs determine physician compensation when the conversion factor (CF), dollars per RVU, is applied to the total RVU. Under the RBRVS, physician payment for services are determined by the following: 1) total RVUs, 2) Geographical Practice Cost Indices (GPCIs), and Conversion Factor (CF).
Outpatient Office Visit Established Patient Level 1 (99211) RVU 0.18 Outpatient Office Visit Established Patient Level 2 (99212) RVU 0.48 Outpatient Office Visit Established Patient Level 3 (99213) RVU 0.97 Outpatient Office Visit Established Patient Level 4 (99214) RVU 1.50 Outpatient Office Visit Established Patient Level 5 (99215) RVU 2.11 Telehealth Outpatient Office Visit Established Patient Level 2 (99212-95) RVU 0.48 Telehealth Outpatient Office Visit Established Patient Level 3 (99213-95) RVU 0.97 Telehealth Outpatient Office Visit Established Patient Level 4 (99214-95) RVU 1.50 Telehealth Outpatient Office Visit Established Patient Level 5 (99215-95) RVU 2.11 Telehealth Outpatient Office Visit New Patient Level 3 (99203-95) RVU 1.42 Telehealth Outpatient Office Visit New Patient Level 4 (99204-95) RVU 2.43 Postoperative Follow Up visit (99024) RVU 0.00 Outpatient Office Consultation Level 4 (99244) RVU 3.02 Telehealth Outpatient Consultation Level 4 (99244-95) RVU 3.02 Outpatient Office New Patient Level 3 (99203) RVU 1.42 Outpatient Office New Patient Level 4 (99204) RVU 2.43 Outpatient Office New Patient Level 5 (99205) RVU 3.17 Telehealth Outpatient Office New Patient Level 3 (99203-95) RVU 1.42 Telemedicine Coding Examples 10 Telehealth Outpatient Office New Patient Level 4 (99204-95) RVU 2.43 Telehealth Outpatient Office New Patient Level 5 (99205-95) RVU 3.17 Initial Inpatient Hospital Care Level 1 (99221) RVU 1.92 Subsequent Inpatient Hospital Care Level 1 (99231-GC) RVU 0.76 Initial Inpatient Hospital Care Level 2 (99222) RVU 2.61 Physician Telephone Evaluation 5-10 min 99441, G2012 RVU 0.48 Physician Telephone Evaluation 11-20 min 99442, G2012 RVU 0.97
1. SGO Telemedicine for Gynecologic Oncology Care During the Covid-19 Pandemic 2. SGO Coding Corner with Dr. David Holtz, MD 3. Medicare Telehealth Frequently Asked Questions 4. Medicare Telemedicine Health Care Provider Fact Sheet 5. From Dr. Shitanshu Uppal FaceTime or WhatsApp: How to implement video calls using FaceTime 6. AMA Quick Guide for Telemedicine
Related Resources
Sgo can help with gynecologic oncology resources.
Have an Idea for SGO’s Gynecologic Oncology Resource Library? Can’t find what you’re looking for? Let us know. We’ll gladly look into it for you.
- 99232 CPT Code, Level 2 Hospital Followup Note –Dummies Guide 2017-2018
A 99232 CPT code explanation, 99232 examples, 99232 example note, 99232 RVU amount, 99232 wRVU / work RVU amount and a 99232 template for EMR.
What is cpt code 99232.
CPT code 99232 is assigned to a level 2 hospital subsequent care (follow up) note. 99232 is the intermediate and most commonly used level of non-critical care daily progress note. When it comes to 99232 documentation is critical, however understanding of the documentation required is even more critical. WorK RVU (wRVU) for cpt code 99232 is of course lower than that for 99233 and higher than that for 99231.
How many work RVU (wRVU) are given for a 99232?
A 99232 CPT code is associated with 1.39 work RVU’s also known as wRVU.
A 99232 = 1.39 wRVU
In general when is a 99232 code appropriate?
When it comes to coding, as always in the day and age of EMR, documentation is key. You would amazed to see just how little documentation is required to ensure all the key criteria. It is critical though that common sense should prevail, there is never anything to be gained from gaming the system with generic documentation.
If a patient is improving or remains stable CPT code 99232 is probably appropriate. If a patient has a new acute problem or worsening of an issue then a 99233 may be appropriate. Often, rounds are made on patients where it is essentially a continue medications and monitoring on an improving patient. These are classic 99232’s.
Often, in the days after a patient is admitted, although management decisions continue to evolve and treatment changes are made, the changes are minimal and the patient is improving. Such as titration of BP or CHF meds in an improving patient. This would be a classic 99232 CPT code type situation. If new issues arise however that you are primarily treating, such as development of renal failure or hypoxia, that require specific medication adjustment and ordering of tests that need to be reviewed 99233 CPT code may be more appropriate. As the patient improves and / or awaiting final stabilization for discharge, CPT code 99232 rather than 99233 would be appropriate.
Example of hospital days where CPT code 99232 may be appropriate as long as the documentation is correct
Admission – Patient with shortness of breath and chest pain, comorbidities present, diagnosed with congestive heart failure and known ischemic cardiomyopathy treated medically, IV meds given, complexity is high.
CPT code 99223
Day 2 – Patient improved, meds changed to PO, home meds restarted, no invasive tests planned, continuing to monitor.
CPT code 99232
Day 3 – Kidney function worsens, meds held and changed appropriately, concern for cardiac output being low, nephrology consulted, situation worsened from prior day.
CPT code 99233
Day 4 – Echo reviewed, cardiac function worse than thought, thinking about right heart cath, dobutamine started on floor, IV diuresis ongoing, discussed with consultants.
Day 5 – Situation improves, renal function stabilizes with inotropic support and renal recommendations, breathing improved, meds regimen stable, labs and CXR stable, patient likely to be discharged in next few days.
Documentation is critical when it comes to a 99232
I can’t say enough that even though this is the most common progress note, documentation is key. It may often be the case that there are new issues and the patient is sick with high complexity. In that case a 99233 may be more appropriate however many people simply write 99232 out of habit. Importantly, under coding is seen as serious an issue as over coding. Unfortunately notes are like a point system where a certain number of points are required for a certain number of categories. That can be advantageous however when it comes to efficiency in documentation for those that understand how it works.

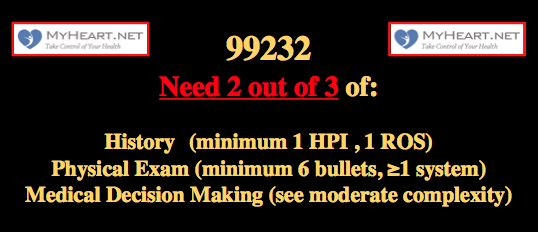
The key Components of a 99232
To bill a 99233 you need at least 2 of the 3 key components .
Expanded and problem focused history
Expanded and problem focused examination
Moderate complexity decision making
See below for a more detailed breakdown of these categories
One may also:
Coordinating care with other providers
Counsel the patient and family
Alternatively a 99232 can be billed on the basis of time as described below.
Time based 99232
The 99232 represent what would typically be 25 minutes of care at the patient bedside.
If 25 minutes was spent with a patient, if there is specific documentation, it is felt that the time alone may justify the 99232. That documentation must include 1) Total time spent (>25mins) 2) Description of the counseling and care coordination 3) State the amount of time that was spent on face to face and also counseling and coordinating specifics of care.

1-3 HPI elements (locations/severity/duration/associated symptoms etc.) and 1 review of systems point.
99232 Examples of interval history:
Chest pain (1) is stable, left chest (2), radiates to neck (3), mild (4). No dyspnea or cough (ROS 1).
Shortness of breath (1) improved after steroids no relation to exertion (2) and mild in nature (3). No chest pain (ROS 1)
These examples easily contain 1-3 elements required for the HPI element of the 99232. If a patient has a stable or improving condition and it is described appropriately this should be easily fulfilled.

6 bullet points from one or more organ systems
1 point includes 3 vital signs reviewed
1 point for general appearance
1 point each for Neck / lung / heart / carotids / abdomen / liver / edema / digits / skin / mental status / neuro etc.
In general I would say include a few organ systems regardless .
99232 examples of detailed exam:
In this cardiac strong exam we have 5 different ‘systems’, we have 9 bullets, this exceeds the required 6.
1 point for these 3 vital signs
BP 136/74, HR 68, 02sat 98% on air (1 point for the 3 vitals)
1 point for this general exam
Laying in bed, mild increase work of breathing
1 point for this mental status exam
Alert and oriented, can follow instruction
2 points for this cardiovascular exam
Regular rhythm, soft systolic murmur, no added sounds (auscultation of heart)
1+ bilateral pitting edema (exam of periphery cardiovascular)
1 point for this exam of neck
JVP 8cm, elevated, bed at 45 degrees
1 points for this respiratory exam
Lungs clear to auscultation bilaterally
2 points for this abdominal exam
Soft and non tender, No masses felt

For a 99232 typically a combination (2 out of 3 needed) of 3 problem points, 3 data points, and documentation of moderate risk.

99232 high complexity decision making – 3 problem points
Minor problem points (maximum of 2) = 1 point
Established problem that is stable or demonstrates improvement =1 point
Established problem that worsens = 2 points
New problem with no further work up planned (max of 1) = 3 points
New problem, with additional work-up needed =4 points
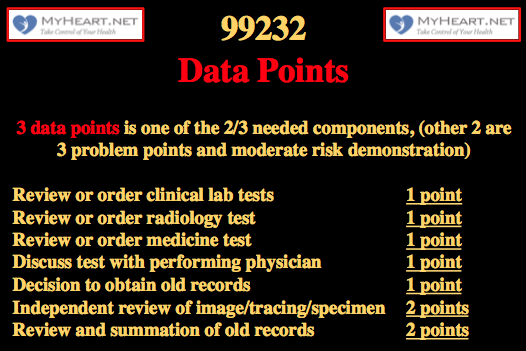
99232 high complexity decision making – 3 Data Points
Review or order labs =1 point
Review or order imaging =1 point
Discuss test with performing physician =1 point
Independently review image / tracing / specimen =2 points
Decide to obtain old records =1 point
Review and summarize old records =2 points

99232 moderate complexity decision making -Demonstration of moderate Risk
Needs one of the following 3 elements
Presenting problems
Diagnostic procedures
Management options
One or more chronic illness with mild exacerbation or progression.
Two or more chronic stable illnesses.
Stress tests
Deep needle biopsy
Cardiovascular imaging studies, with contrast, with no identified risk factors
Obtain fluid from body cavity (LP, thoracentesis, etc.)
Minor surgery
Elective major surgery
Prescription drug management
IV fluids with additives
Closed treatment of fracture
Comprehensive templates for 99232
Presented is a comprehensive template for a 99232. People will argue that its overkill and takes a lot of time, however I disagree. If the stated elements are reviewed it clearly improves patient care, as often ignored elements will be reviewed. The documentation is comprehensive but in reality not overly time consuming in the era of EMR, particularly if auto-population is used and you are familiar with the patient. If a significant portion of these elements is followed you will much more than fulfill the documentation criteria for a 99232. For those learning the specifics of documentation I would suggest starting comprehensive like this then when you feel comfortable the note can be trimmed significantly and tailored to needs.
Interval HPI;
(Describe treating issue with 1-3 HPI points, and add at least 1 review of system point)
( if new significant problem consider 99233 and ensure fulfillment of documentation )
Lab review; (between this and tests, need only 3 data points)
(Pull in lab values if desired)
(Comment on any changes on the review)
Test Review; (between this and labs, need only 3 data points)
(Pull in radiology testing) New radiology tests include
(CXR reading and review) CXR was reviewed and demonstrated
(EKG 12 lead reading and review) 12 lead EKG was reviewed and demonstrated
(Telemetry review and comment) Telemetry was reviewed and demonstrated
(Pull in meds if required)
Physical Exam; (remember need only 6 bullet points from the following)
(Pull in BP, HR, temp, 02sat)
(Laying in bed / sitting in chair / ambulating)
(Comfortable / uncomfortable / other comment)
(Alert and oriented, able to answer questions)
(JVP is not elevated, carotid exam normal)
(Regular rate and rhythm, no murmurs noted, no added heart sounds, normal apical pulsation)
(2+ radial pulses bilateral, 2+ femoral/tibial pulses bilaterally)
(no edema in the lower extremities)
(no clubbing or cyanosis)
(Lungs clear to auscultation bilaterally, respiratory effort normal)
(Abdomen soft and non tender, normal bowel sounds)
(No new rashes or ulceration noted)
(Problem list being actively managed)
( If significant new problems interval – work up ordered, treatment started consider 99233 and fulfill other criteria for that )
(Problem 1 – stable / treating, – management)
(Problem 2 – stable / treating, – management)
(Problem 3 – stable / treating, – management)
(Problem 4 – stable / treating, – management)
Comprehensive cardiology centered template example for 99232 – see below for a detailed breakdown and discussion
Chest pain has improved, still some intermittent instances of chest pain.
No shortness of breath, nausea or diaphoresis.
Lab review;
Labs reviewed
Troponin remained negative
Test Review;
CXR was reviewed and stable
12 lead EKG was reviewed and normal sinus rhythm at a rate of 70
Telemetry was reviewed and demonstrated sinus rhythm rate 80-110
Medication list or can simply say was reviewed
Physical Exam;
BP 100/70, HR 90, temp 98.0, 92% 02sat on 4 liters
Alert and oriented and able to answer questions
Laying in bed
No increased work of breathing
JVP normal at 8cm at 45degrees, carotid upstroke normal
Cardiac exam, regular rhythm, no murmurs noted
2+ radial pulses bilateral
Lungs clear bilaterally, respiratory effort normal
Abdomen soft and non tender
Chest pain – stable, markers negative
Hypertension, chronic, controlled
Diabetes Mellitus, controlled
Smoker – nicotine patch
Ongoing Issues
Chest pain, central chest, atypical in nature, markers negative, echocardiogram pending, continue aspirin.
Hypertension – currently normotensive, continue calcium channel blocker
Diabetes Mellitus – controlled, basal bolus insulin, readings acceptable, pharmacy co-management
Smoking – counseled, nicotine patch placed
Detailed Breakdown of the 99232 note template and example.
The example above is a relatively extensive documentation, it would take some people a long time to do that and others could run through it relatively quickly. If methodically done, be in an efficient manner.
By no means is all the documentation above needed. The note basically scores top points in every requirement, and remember only 2 out of the 3 are needed.
Interval HPI
This has already hit the 1-3 HPI points required . There are 3 ROS points here, exceeding the 1 required . Theoretically only 1 of the other 2 categories (physical exam and moderate complexity decision making) is now needed.
The review of the labs contribute a point to the data point section of the medical decision making section. Remember, 3 data points are needed as part of the 2 of 3 requirements for moderate complexity decision making. Remember, a new significant problem with additional work up planned fulfills 4 points and qualifies for high risk and so in that setting 99233 may be more appropriate .
Personally reviewing the radiology test CXR is 2 points. Independent review of the EKG is 2 points (If we had decided to review old records and summarized that would have been 2 points). Later we order an echo, that’s a further point. We had already reviewed the lab above, that’s a further point. In total here we have 6 data points that exceeds the 3 data points required for the 99232. That’s already one of the 2 requirements of the moderate medical decision making out the way. Remember it has to be 2 out of the 3 of: 3 problem points, 3 data points and moderate risk.
BP 100/70, HR 90, temp 98.0, 98% 02sat on 2 liters (1 point)
Alert and oriented and able to answer questions (1 point)
Laying in bed , No increased work of breathing (1 point)
JVP normal at 8cm at 45degrees, carotid upstroke normal (1point)
Cardiac exam, regular rhythm, no murmurs noted (1 point)
2+ radial pulses bilateral (1 point)
Lungs clear bilaterally, respiratory effort normal (1 point)
Abdomen soft and non tender (1 point)
Remember that a total of 6 bullets are needed. 3 vital signs are 1 point and general appearance is 1 point. In the exam above we have a total of 8 points, it easily fulfills requirements.
Chest pain – stable, markers negative (1 point)
Hypertension, chronic, controlled (1 point)
Diabetes Mellitus, controlled (1 point)
Smoker – nicotine patch (1 point)
These 4 stable points are ok as they are issues that significantly impact treatment.
Our documentation here is basically worth 3 problem points, remember we only need 3. 1 points each for the established chronic stable issues up to a maximum of 2. And 1 point for the new problem, chest pain that is improving.
Ongoing Issues
Chest pain, central chest, atypical in nature, markers negative, echocardiogram pending, continue aspirin.
In the section above we have simply bolstered our documentation above. We have laid out the problems and demonstrated the further work up planned. We have reported the management of the chronic issues. We have documented tests planned and discussions had.
Specifics (optional, but count as documentation points, I make a routine of documenting these)
Discussions: Discussed with patient who understands issues and daughter at bedside
Review: General medicine and PT note reviewed
Tests: Echo ordered and pending
Code: Remains Full Code
The discussion with the other physicians involved and also the discussion with the family is a supporting factor for complexity. The review of the medical and the PT notes can act as a point in data. The ordering of the new echo acts as a data point also.
Brief note example that fulfills the criteria for a 99232
I’m not a fan of minimalist notes, I think it can breed complacency and doesn’t help with the thought process. The following shows however that when sticking to the criteria for a 99232 we can still achieve what we need to with a minimal note.
Interval history
Chest pain has improved, still some intermittent chest pain.
No shortness of breath or dizziness.
2 interval HPI points, 2 ROS points. (Only need 1-3 HPI points and 1 ROS point)
Objective points
BP 100/70, HR 90, temp 98.0, 98% 02sat on 2 liters, Alert and oriented, Laying in bed , JVP normal at 8cm at 45degrees, carotid upstroke normal, Cardiac exam, regular rhythm, no murmurs noted , 2+ radial pulses bilateral, Lungs clear bilaterally, respiratory effort normal, Abdomen soft and non tender
Theoretically we could stop here, we have 2 of the 3 main sections with all criteria fulfilled, interval HPI has the necessary points and the physical exam has 8 bullets, remember only 6 needed. This highlights how knowledge of what’s required can allow focus on main issues if that is the aim. In reality the note will continue thought.
Assessement
Chest pain – stable, markers negative, EKG reviewed and no changes noted.
Fulfilled the 3 problem points needed. The EKG and the lab review acts as data points for the moderate complexity decision making also. In theory this is all that’s needed, you could even take out the physical exam section and still have fulfilled 2/3 requirements as needed.
Chest pain – Markers negative, trend another set, echo pending.
HTN – continue calcium channel blocker for HTN.
Diabetes Mellitus – continue basal bolus insulin, pharmacy co-management.
Smoking –nicotine patch placed
This note was very short, but still way over the requirement in terms of points needed, essentially its point system dense and easily fulfills the documentation needs for a 99232.
Even briefer note example that fulfills the criteria for a 99232
Chest pain has mostly improved.
No shortness of breath.
1 interval HPI point, 1 ROS. (1-3HPI needed, 1 ROS needed)
Technically the exam isn’t required!
3 data points can be; EKG reviewed no significant ST-T changes (2 points). Cardiac markers reviewed and negative.
3 data points already, (remember now we only need either moderate complexity risk or 3 problem points to complete the 2 out of 3 aspects of moderate complexity decision making)
Chest pain – trend markers, order echo
Diabetes – controlled
HTN – controlled
(2 or more stable chronic illnesses is moderate risk, the other classic for the 99232 is one or more chronic illness, with mild exacerbation, progression, or side effects of treatment)
This note was very very short, but still easily met the requirement in terms of points needed, essentially its highly point system based and despite the brevity of the note fulfills the documentation needs for a 99232.
- Cardiology Coding Center
- Combined Right and Left Heart Catheterization CPT Codes and RVU
- Coronary Intervention CPT Codes and RVU
- Echocardiography CPT Codes and RVU
- Left Heart Catheterization CPT Codes and RVU
- Left Heart Catheterization Miscellaneous CPT Codes and RVU
- Right Heart Catheterization CPT Codes and RVU
- Structural Heart Intervention CPT Codes and RVU
- Coronary Artery Imaging CPT Codes and RVU
- 99233 CPT Code, Level 3 Hospital Followup Note –Dummies Guide 2017-2018
- Newsletters
- FAC Articles

Keep your critical coding and billing tools with you no matter where you work.
Create your Find-A-Code account today!
Find-A-Code Articles, Published 2023, September 12
Documenting and reporting postoperative visits.
by Aimee L. Wilcox, CPMA, CCS-P, CST, MA, MT Sep 12th, 2023
CPT® 99024 was introduced by the American Medical Association (AMA) with an effective reporting date of January 1, 2013. The associated code description is as follows:, 
“Postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure”
To fully understand this code description, one must also understand the definition of the global surgical package, which CPT® describes as:
Of note, Medicare published their own definition of the global surgical package (see Chapter 12, Section 40.1 of the Medicare Claims Processing Manual-Pub. 100–04), which differs from the CPT® surgical package. The surgical package policy applied to an individual claim is determined by the patient’s insurance company’s published policies.Payers without published policies must adhere to the CPT® guidelines.
Prior to 2017, pre/postoperative services with a zero-dollar charge, were not submitted on claims. Because of this, a proper analysis of the quality and quantity of services that make up a global surgical package was not possible, as there was a deficit in the data that showed postoperative services. In 2015, Medicare proposed a change in the global surgical package to return all surgical procedures to a zero-day global period to promote a more accurate valuation of surgical services through coding data. However, Section 523(a) of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) (Pub. L. 114–10, enacted April 16, 2015) added section 1848(c)(8)(A) of the Act, prohibited the Secretary from implementing this change.
Instead, on January 1, 2017, Medicare required specific large provider groups, identified by them, to report via claim, all preoperative and postoperative services provided during the global surgical period. Although the requirement was only specific to certain large provider groups and not all Medicare providers, all Medicare contracted providers were encouraged to do likewise. This policy was strategic to facilitate a more accurate valuation of more than 4,000 surgical procedures assigned a 0, 10, or 90-day global period.
Each surgical procedure is assigned either a 0, 10, or 90-day global period; however, according to the global surgical package, the day of the procedure is considered bundled into the procedure for 0-day and 10-day global periods, which means technically the 10-day global period is actually an 11-day global period (day of the procedure and the 10 days following the procedure). For 90-day global periods, which are considered to be major surgical procedures, the day prior to the surgery, the day of the surgery, and 90 days following the surgery, are included in the global period, essentially making a 90-day global period actually a 92-day global period.
Preoperative services performed on the day of a 0-day or 10-day surgical procedure are bundled into the procedure itself. As an example, let’s review the following patient scenario:
Scenario: A patient has an appointment to have their nails trimmed in the office. The physician documents a history related to the patient’s chronic conditions and how they impact his ability to trim his own nails, examines the patient’s nails, and determines there are 8 that need to be trimmed. The provider documents the procedure where the nails are trimmed, including the method used, the nails trimmed, and the outcome and any instructions on nail care to the patient.
Code: 11721 - Debridement of nail(s) by any method(s); 6 or more is reported but not anEvaluation and Management (E/M) service code. The reason being, is that this was a scheduled procedure and all of the history and exam were related to why the patient has the condition, needs the service performed, and the actual performance of the service, all of which are considered the preoperative workup included (bundled) into the service itself.
Same Day Surgeries
Currently, there are 1,190 surgical procedures with a zero-day global period, 468 surgical procedures with a 10-day global period, and 3,743 major surgical procedures with a 90-day global period. Code 99024 is used to report postoperative services, beginning with any postoperative care provided on the day of the surgery (after the surgery has been performed) and each visit thereafter, where postoperative care is provided through the end of the assigned global period. For same day surgeries (SDS), that means all care related to admitting the patient, postoperative care up until discharge, and inclusive of the discharge services. The same applies to admission and discharge services, as well as inpatient E/M services provided to a patient in the inpatient hospital setting. Facilities who accurately report all postoperative services with 99024 during the global period would also report 99024 for any admission and discharge services, instead of the usual CPT codes for those services, and all are bundled into the surgical package, unless specific surgical or patient care for other conditions or complications is provided that is beyond what is covered in the surgical package.
However, it should be noted that if the surgeon is billing for Evaluation and Management services, during the global period, that are unrelated to the surgical procedure and global period, and the documentation supports the clear distinction of these services, the provider may report the E/M service with modifier 24 to specify it is a distinct and separately billable service provided during the global period.
Splitting Surgery and Postoperative Care
Occasionally, the surgeon who performs the surgery is not available to perform the preoperative and postoperative care. This can be because pre and postoperative services are provided in a different state than the surgeon resides and the patient has returned home after surgery to get postoperative care by their own physician, or another reason exists. Be sure to check individual payer policies related to splitting the surgical global package components to ensure coverage, medical necessity, documentation requirements, and modifier use for reporting claims.
When the global surgical package is split between providers for Medicare beneficiaries, each provider will report the surgical CPT code and the modifier that applies to the services they are providing and in the narrative box on the claim, will provide the details of the services and service dates they are providing to the patient. Novitas, and other Medicare Administrative Contractors (MACs) have provided published documents to review this process in detail.
Documentation
Clear documentation is very important in ensuring accurate reimbursement for services rendered, whether for the entire global surgical package or when it has to be split between providers. An operative report that clearly describes the pre/postoperative diagnosis, name of the procedure, and the details of how it was performed, is a must have for claims submission and medical necessity. Likewise, each postoperative report should contain language that indicates the patient is presenting for a postoperative visit, including the postoperative date (e.g., POD#7, status post day 7) and the surgical procedure they had done, including the date the procedure was performed. This facilitates proper coding for the global period and an accurate reflection of postoperative care provided to the patient following surgery.
Additionally, be sure to document any postoperative care, such as:
- Patient complaints, symptoms, or complications directly related to the surgical procedure.
- Examination of the patient, especially the body area or organ system impacted by surgery.
- Medications or treatments that have been prescribed, including pain management.
- Follow-up testing or imaging ordered to check the patient’s status after surgery.
- Any conditions, symptoms, or treatments that are unrelated to the surgical procedure that may qualify for appending modifier 25 to the E/M service.
Separately Reportable E/M Service on the Day of a Postoperative Visit by the Same Provider
When a postoperative visit turns into an E/M service for an unrelated condition, the provider may be eligible for payment if the documentation supports a separately, identifiable E/M service as well as the postoperative visit service. Providers often combine these two services in a single report; however, to ensure accurate payment and reduce confusion that may occur during an audit, we recommend either documenting the postoperative care first and in the same note, just separated from it, document a complete E/M service note as well for the unrelated problem. Providers may also choose to simply document two separate reports, one for the postoperative visit and another for the separately identifiable E/M service on the same date. To ensure the E/M service is paid, when the documentation qualifies the service, report modifier 24 (unrelated E/M by the same physician during the postoperative period) with the E/M service code to clarify it is an unrelated service. If supporting documentation is requested by the payer, be sure to send both reports, the postoperative note and the E/M service note for clarity.
Of note, there is no NCCI edit between 99024 and E/M service codes indicating that if both a postoperative visit and an unrelated E/M service are performed on the same day by the same physician/provider, they may be reported on the same claim; however, be sure to append modifier 24 to the E/M service code to instruct the payer that the provider documentation supports unbundling the E/M service from the global period for payment.
References/Resources
About aimee l. wilcox, cpma, ccs-p, cst, ma, mt.

Documenting and Reporting Postoperative Visits. (2023, September 12). Find-A-Code Articles. Retrieved from https://www.findacode.com/articles/documenting-reporting-postoperative-visits-37422.html
Article Tags (click on a tag to see related articles)
Thank you for choosing Find-A-Code, please Sign In to remove ads.


Emily Ratajkowski's Hottest Shots To Celebrate Her 33rd Bday!

Guess Who This Adorable Kid Turned Into!

Dad Blocks Superintendent from Daughter at Graduation, Motives Questioned

See Sommer Ray's Shining Shots In Her Gold Metallic Bikini ... Golden Girl!

Taylor Swift's Concert Crashed By Mysterious Shadowy Figure Watching from Above
Pa school crossing guard arrested, accused of giving kids vapes, edibles, school crossing guard accused of giving kids vapes, edibles arrested & charged.
A Pennsylvania crossing guard has drawn huge outrage -- this after she was arrested for allegedly giving drugs to middle schoolers and even smoking weed with one of them.
Cops in Delaware County handcuffed 26-year-old Kiara Lee , a Penn Wood Middle School employee, Tuesday ... after reports emerged witnesses had seen her giving children e-cigarettes and weed edibles.
There were loads of other similar claims against Lee -- one student's guardian said Lee had been giving their child vapes and marijuana edibles.
That's not all -- there are also claims Lee stayed in touch with a student through text messages, where they'd swap stories about munching on edibles.
Darby Borough Chief Joseph Gabe didn't mince words as he stated the obvious ... "While marijuana might not seem like a big deal to some folks in the community, I think we can all agree that crossing guards should not be providing narcotics -- even if it is 'just' marijuana -- to our kids."
Lee's facing serious charges: 2 felony counts of drug possession with intent to deliver, 2 misdemeanor counts of corruption of a minor, and 2 misdemeanor counts of possession of marijuana.
She apparently couldn't post the $20,000 bail, so now she's cooling her heels in the Delaware County jail. She's got a date in court for a preliminary hearing on June 14.
- Share on Facebook
related articles

Sean Kingston Surfaces in Florida After Jail Release, Mom & Safaree Visit
Old news is old news be first.
- Live In The D
- Newsletters
English soccer club announces partnership with Visit Detroit
Burnley fc says visit detroit will be official us destination partner of club.
Keith Dunlap , Digital Content Team, Graham Media Group
Cheers to a new partnership between an English soccer club and a prominent Detroit economic development organization.
Burnley FC has announced a “long-term” collaboration with Visit Detroit that will make the organization the official U.S. destination partner of Burnley FC.
Recommended Videos
While competing at The Soccer Tournament upcoming in Cary, North Carolina, Burnley will have Visit Detroit’s logo on its jerseys.
“We are delighted to begin this new journey with Visit Detroit in this remarkable partnership,” said Marcus Mellor, head of commercial at Burnley FC, in a statement. “Football transcends geographical boundaries, and I’m pleased that through this collaboration we can strengthen our ties with U.S. communities and fly the Clarets flag stateside as we celebrate the passion for the beautiful game.”
Claude Molinari, president and CEO of Visit Detroit, added in the statement that “football wouldn’t be football without Burnley FC.”
“For more than 140 years, Burnley FC has been marching forever forward, and Visit Detroit is excited to join their campaign for promotion and ascendancy in English and global football,” he said. “Together, we will showcase the passion of our communities, forging a powerful connection between Detroit and the beautiful game.”
Copyright 2024 by WDIV ClickOnDetroit - All rights reserved.
About the Author
Keith dunlap.
Keith is a member of Graham Media Group's Digital Content Team, which produces content for all the company's news websites.
Click here to take a moment and familiarize yourself with our Community Guidelines.
Advertisement
How does four-star jaelyne matthews feel about rutgers football after his ov, share this article.
Jaelyne Matthews is in the midst of a busy time in his recruitment. The four-star offensive lineman just had an official visit to Rutgers over the weekend and now has official visits lined up for Miami and Tennessee .
The official visit for Matthews at Rutgers ran Saturday through Monday because he attended prom on Friday night. Most of the recruits on campus saw their official visits run from Friday through Sunday afternoon.
Matthews is a prominent national recruit. The Toms River North (Toms River, New Jersey) offensive tackle is the No. 93 player in the nation in the ESPN 300. He is the second-ranked recruit by ESPN in New Jersey’s class of 2025.
“This weekend went well. I feel as though the coaching staff recruiting me and (they were) making my girlfriend and her family feel at home,” Matthews told Rutgers Wire on Tuesday night.
Following his freshman season, Matthews was first offered by Rutgers.
Miron Gurman shoots up the recruiting rankings after Rutgers football commitment
Three-star edge taeshawn alston previews his upcoming rutgers football official visit.
Matthews said that one thing he wanted to know over the weekend from Rutgers was that he was a priority for them.
The Scarlet Knights are in a crowded recruitment that includes some of the top programs in the nation.
“Yes, they for sure did make me a priority,” Matthews said.
He posted an update about his Rutgers recruitment over the weekend.
In terms of where Rutgers is in his recruitment, Matthews said that the weekend was good and re-inforced his feelings about the direction of the Scarlet Knights. Last year, Rutgers finished with a winning record for the first time since 2014.
Where does Rutgers football rank in the ESPN FPI?
Offered by colorado and miami, raedyn bruens is all in - 'i'm 100% committed to rutgers'.
They beat Miami in the Pinstripe Bowl to cap off the season.
“They pretty much stayed the same,” Matthews said of where things stand with Rutgers. “I feel as though Rutgers is a great program and they are going to do great things and I wish them the best of luck.”
Most Popular
How do the big ten recruiting classes rank, espn analyst greg mcelroy names his five candidates for big ten conference expansion, rutgers football now has a top-10 recruiting class in the nation, barstool legend 'frank the tank' features former rutgers football star eric legrand, no surprise but rutgers women's basketball recruit autumn fleary makes the 'super 60' list.
Please enter an email address.
Thanks for signing up.
Please check your email for a confirmation.
Something went wrong.
How to Code for Telehealth, Audio-Only, and Virtual-Digital Visits
Learn how to accurately get paid for telemedicine services with medical codes for telehealth, audio-only, and virtual-digital visits.
Looking for additional telemedicine coding resources?
Coding for Telehealth Visits
Note: These tables are informational, not advisory. The AAFP recommends that physicians verify each payer's policy and ask patients to verify their coverage ahead of appointments.
How do I code a new or established patient telehealth office visit that uses audio-video communications technology?
* Elevance's policies vary by state; contact your provider-relations representative.
Coding for Audio-only Visits
How do i code an audio-only visit for a new or established patient .
CPT Codes: 99441-99443
Audio-only scenario notes
Medicare requires audio-video for most office visit evaluation and management (E/M) services (CPT codes 99202-99215) telehealth services. Audio-only encounters are allowed for certain services. Eligible services may be found on the Medicare Telehealth Services list. Medicare allows audio-only telehealth services for office visit E/M services (CPT codes 99202-99215) for the treatment of mental health conditions.
UHC states they will consider payment for eligible audio-only services listed in Appendix P of the CPT book. Eligible services must be reported using either POS 02 or 10 and include the -93 modifier. CPT codes billed with modifier -93 that are not in Appendix P will not be considered for payment.
Private payers vary on covered telehealth services. Check with your provider relations representatives for each payer’s telehealth policy and covered telehealth services.
CMS will cover telephone evaluation and management (E/M) services (CPT codes 99441-99443) through the end of calendar year 2023. Other services that may be provided via audio-only are available on the Medicare Telehealth List.
Telephone E/M services are provided to a patient, parent, or guardian and do not originate from a related E/M service within the previous seven days and do not lead to an E/M service or procedure within the next 24 hours or soonest available appointment.
The following codes may be used by physicians or other qualified health professionals who may report E/M services:
- 99441: telephone E/M service; 5-10 minutes of medical discussion
- 99442: telephone E/M service; 11-20 minutes of medical discussion
- 99443: telephone E/M service, 21-30 minutes of medical discussion
Telephone E/M services should not be reported when the time spent on the telephone is captured in other services reported, such as:
- if CPT codes 99421-99423 have been reported by the same physician in the previous seven days for the same problem,
- when CPT codes 99339-99340 and 99374-99380 are used for the same call,
- during the same month with CPT codes 99487 and 99489, and
- when performed during the same service period at CPT codes 99495-99496.
- Self-funded plans can develop their own policies and may opt out of some cost-sharing waivers. Similarly, Medicaid policies are established at the state-level. The AAFP recommends reaching out to your provider relations representatives or Medicare Administrative Contractors (MACs) to verify policies.
Coding for Virtual-Digital Visits
How do i code an e-visit (cpt 99421-99423) for an established patient .
CPT Codes: 99421-99423
How do I code a virtual check-in (HCPCS codes G2012 and G2010) for an established patient?
HCPCS Codes: G2012, G2252, G2010
Virtual/Digital Scenario Notes
- Patient consent is required and may be obtained either before or at the time of service.
- Virtual check-ins and e-visits must technically be initiated by a patient; however, physicians and other providers may need to educate beneficiaries on the availability of the service prior to patient initiation.
- There are no POS or modifier requirements for virtual check-ins or e-visits. Use the POS used for typical services.
Virtual Check-in (HCPCS Code G2012, G2252)
- These are brief conversations with a physician or other clinician to determine if an in-person visit is necessary.
- The communication cannot be related to a medical visit within the previous seven days and cannot lead to medical visit within the next 24 hours (or soonest appointment available).
- Physician or other clinician may respond to patient by telephone, audio/video, secure text messaging, email, or patient portal.
- HCPCS code G2010 can be used when a captured video or image (store and forward) is sent to the physician. The physician must follow up with the patient within 24 business hours. The consultation must not originate from an evaluation and management (E/M) service provided within the previous seven days or lead to an E/M service within the next 24 hours (or soonest available appointment).
E-Visits (online digital evaluation and management services)
- These are non-face-to-face, patient-initiated communications with the physician through an online patient portal. The communications can occur over a seven-day period, and the exchange must be stored permanently.
- Cumulative time includes review of the initial inquiry, review of patient records pertinent to the assessment of the patient’s problem, personal interaction with clinical staff focused on the patient’s problem, development of management plans (including generation of prescriptions or ordering of tests), and subsequent communication with the patient. Communication can occur through online, telephone, email, or other digitally supported communication
Physicians and other clinicians who may independently bill Medicare for E/M services can use the following codes:
- 99421: Online digital evaluation and management service, for a patient, for up to 7 days, cumulative time during the 7 days; 5-10 minutes
- 99422: Online digital evaluation and management service, for a patient, for up to 7 days, cumulative time during the 7 days; 11-20 minutes
- 99423: Online digital evaluation and management service, for a patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes
E-visits should not be billed on the same day the physician reports an office visit E/M service (CPT codes 99202-99205 and 99211-99215) for the same patient. Additionally, e-visits should not be billed when using the following codes for the same communication:
- 99339-99340
- 99374-99380
- 99487 and 99489
- 99495-99466
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Next, complete the following calculations: Work RVUs per session ÷ Visits per session = Work RVUs per visit. 16.88 ÷ 10 = 1.69. Workdays per year x Visits per day = Visits per year. 220 x 20 ...
Consult follow-up visits are beneficial to patient and the primary service because the consultant's expertise can be applied to new test results and changes in the patient's condition. ... and when combined with a level 5 new outpatient visit (3.17 wRVUs), you can generate a whopping 5.27 wRVUs (7.91 total RVUs) for that visit. I use this ...
The Medicare Physician Fee Schedule Final Rule (2023 Final Rule) includes both increases and decreases in work RVU values for E&M services provided in hospital and nursing facility settings. Generally, the most used billing codes (99232, 99233, 99308, and 99309) within this subset are all going to realize double digit increases in work RVUs.
As a result of the changes to medical decision making and time-based coding, the RUC revised the 2021 relative value units (RVUs) for office visit E/M codes. Most of the values increased, yielding ...
RVU stands for relative value unit. It is a value assigned by CMS to certain CPT ® and HCPCS Level II codes to represent the cost of providing a service. An RVU is made up of three components: physician work, practice expense, and malpractice. Medicare payments are determined by RVUs multiplied by a monetary conversion factor and a geographic ...
The reimbursement per RVU is being adjusted for 2021. The budget neutrality adjustment, as required by law, accounts for changes in RVUs including significant increases for E/M visit codes. CY 2021 PFS conversion factor is $32.41, a decrease of $3.68 from the CY 2020 PFS conversion factor of $36.09. Represents 10.2% reduction in reimbursement.
Increasing RVUs for follow-up visits, considering their complexity and the time they entail, which are not comparable to a general medical visit. Abandoning RVUs and substituting other measures (eg, the number of new patients—at least 2 per half-day sessions in addition to follow-up visits) because the downstream effect of a new patient is ...
The 2023 CMS revisions to RVU weighting factors and methodology include positive changes related to Evaluation and Management visits, allowing either time or medical decision-making as factors in visit level. In addition, under the 2023 changes, many prolonged service codes were added, deleted, or modified.
New Patient Office/Outpatient Visits wRVU New patient Level 2 (99202) 15-29 min 0.93 New patient Level 3 (99203) 30-44 min 1.60 New patient Level 4 (99204) 45-59 min 2.60 New patient Level 5 (99205) 60-74 min 3.50 Established Patient Office/Outpatient Visits Established patient Level 1 (99211) nursing level 0.18 ...
2.42 RVU $84.44 2.42 RVU Video visit 99213-95 $92.47 2.65 RVU $68.04 1.95 RVU $68.04 1.95 RVU Phone E/M 99441-95 $56.88 1.63 RVU $36.29 1.04 RVU $36.29 1.04 RVU. ... (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the
A 99233 CPT code explanation, 99223 examples, 99233 example note, 99233 RVU amount, 99233 wRVU / work RVU amount and a 99233 template for EMR. What is CPT Code 99233? CPT code 99233 is assigned to a level 3 hospital subsequent care (follow up) note. 99233 is the highest level of non-critical care daily progress note.
Work, practice expense and liability relative value units (RVUs) are updated annually through Medicare Physician Fee Schedule rulemaking. In response to the recently finalized 2023 Medicare Physician Fee Schedule and related addenda, the ACC developed a new Physician Fee Schedule Calculator.This tool allows clinicians and practice managers to estimate the impacts of the slated changes to ...
Postoperative Follow Up visit (99024) RVU 0.00 Outpatient Office Consultation Level 4 (99244) RVU 3.02 Telehealth Outpatient Consultation Level 4 (99244-95) RVU 3.02 Outpatient Office New Patient Level 3 (99203) RVU 1.42 Outpatient Office New Patient Level 4 (99204) RVU 2.43
CPT code 99232 is assigned to a level 2 hospital subsequent care (follow up) note. 99232 is the intermediate and most commonly used level of non-critical care daily progress note. When it comes to 99232 documentation is critical, however understanding of the documentation required is even more critical. WorK RVU (wRVU) for cpt code 99232 is of ...
Article. Relative value units (RVUs) are the basic component of the Resource-Based Relative Value Scale (RBRVS), which is a methodology used by the Centers for Medicare & Medicaid Services (CMS) and private payers to determine physician payment. RVUs do not directly define physician compensation in dollar amounts.
The national average for family physicians' usage of the level 4 code (99214) is slowly increasing and is approaching 50% of established patient office visits (it's now above 50% for our Medicare ...
TCM Relative Value Units Add Up. TCM codes reward patient care with work relative value units (RVUs) — a major component of the formula that generates provider payment. Per AAPC's Work RVU Calculator, 99495 (moderate complexity TCM) has an RVU of 2.11 and 99496 (high complexity TCM) has an RVU of 3.05.
by Aimee L. Wilcox, CPMA, CCS-P, CST, MA, MT Sep 12th, 2023. CPT® 99024 was introduced by the American Medical Association (AMA) with an effective reporting date of January 1, 2013. The associated code description is as follows:, "Postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a ...
RVUs 2021 Proposed Work RVUs Work RVU Difference Work RVU % Change 2020 Non-Facility PE RVUs 2021 Proposed Non-Facility PE RVUs Non-Facility RVU Difference Non-Facility RVU % Change 99201 Office/outpatient visit new 99202 Office/outpatient visit new 0.93 0.93 0.00 0% 1.12 1.12 0.00 0% 99203 Office/outpatient visit new 1.42 1.60 0.18 13% 1.48 1. ...
The Medicare allowable reimbursement for this level of care is $183.19. Effective January 1, 2021, this level of care requires high complexity MDM or a total of 40 - 54 minutes spent before, during and after the visit on the date of the encounter.
Follow-up After Emergency Department Visit for Substance Use (FUA) This HEDIS ® measure evaluates the percentage of emergency department (ED) visits for members 13 years of age and older with a principal diagnosis of substance use disorder (SUD), or any diagnosis of drug overdose, who had a follow up visit for SUD during the measurement year ...
Sean Kingston Surfaces in Florida After Jail Release, Mom & Safaree Visit SCHOOL CROSSING GUARD ACCUSED OF GIVING KIDS VAPES, EDIBLES Arrested & Charged!! 6/6/2024 8:05 AM PT
Scheduled follow-up visit for multiple significant but stable problems. Remember to show extra work to justify 99214 vs. 99213. New headache, dizziness, abdominal pain, or dyspnea on exertion.
Cheers to a new partnership between an English soccer club and a prominent Detroit economic development organization. Burnley FC has announced a "long-term" collaboration with Visit Detroit ...
AsiaSoutheast Asia. US vies to reset Cambodia ties with Pentagon chief's visit to China ally. US Defence Secretary Lloyd Austin landed in Phnom Penh for a one-day visit on Tuesday en route from ...
Kristian Dyer. June 6, 2024 12:01 am ET. Jaelyne Matthews is in the midst of a busy time in his recruitment. The four-star offensive lineman just had an official visit to over the weekend and now has official visits lined up for Miami and . The official visit for Matthews at ran Saturday through Monday because he attended prom on Friday night.
The physician must follow up with the patient within 24 business hours. ... for up to 7 days, cumulative time during the 7 days; 21 or more minutes ... E-visits should not be billed on the same ...