- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- E/M Coding and Billing Res...
- Office/Outpatient E/M Visi...

Office/Outpatient E/M Codes
2021 e/m office/outpatient visit cpt codes.
The tables below highlight the changes to the office/outpatient E/M code descriptors effective in 2021.
More details about these office/outpatient E/M changes can be found at CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes.
All specific references to CPT codes and descriptions are © 2023 American Medical Association. All rights reserved. CPT and CodeManager are registered trademarks of the American Medical Association.
Download the Office E/M Coding Changes Guide (PDF)

10 Efficient Medical Billing and Coding Practices to Maximize Reimbursement
Joseph muscente.
May 16, 2024
Navigating the maze of medical billing is challenging at best, but mistakes and inefficiencies can be costly. Each year, healthcare providers lose billions of dollars due to coding mistakes and other poor billing practices.
Mastering the art of medical billing is essential to making sure your practice gets the reimbursements due for services provided and to ensure your practice’s financial health. Accurate medical billing also contributes to an overall positive patient experience, as patients can count on clarity in their financial responsibilities.
There’s no one-size-fits-all formula for ensuring a clean claim rate of 95% or higher, though. Rather, it takes a multifaceted, nimble, collaborative approach by an organization’s entire team. There are, however, things all healthcare practices can do to ensure the best possible outcomes.
Here are 10 effective coding strategies to make sure your healthcare practice maximizes reimbursements to ensure financial viability in an increasingly challenging healthcare landscape:
1. Review your process regularly. Medical billing is a constantly evolving process due to changes in legislation, fee schedules, procedure coverages and other items that affect reimbursements. Set a schedule to review your contracts with insurance companies as well as Medicare and Medicaid regulations on a regular basis, and make adjustments to your procedures and documents as necessary.
Also, regular audits of your billing and coding practices serve as a crucial checkpoint. They allow you to identify areas of weakness and areas for improvement.
2. Collaborate and communicate with all parties involved. Establishing clear communication channels between healthcare providers, coders, administrative staff and other team members is essential. It fosters a collaborative environment that not only reduces errors and streamlines workflow but also ensures patients aren’t blindsided by unexpected charges .
Continuous education and training initiatives ensure all team members remain current with evolving practices and regulations and feel empowered to perform at their best. Regular evaluation of metrics, such as your clean-claims ratio, is essential too. Sharing these benchmarks with staff cultivates a sense of ownership and accountability, encouraging everyone to actively contribute to process improvements and adapt as necessary.
3. Get basic. Recording patient information, such as their name, address and date of birth, accurately is crucial to maximizing reimbursements. Typos and missing or incomplete information can lead to delays, denials and overall frustration. In fact, according to Northwest Career College, as many as 20% of claims are denied due to inaccurate or outdated patient information .
4. Verify insurance. Getting a patient’s insurance information correct is paramount. That means verifying there haven’t been any changes at each visit, even if they visit frequently. Also, because coverage can change anytime, make sure to check eligibility for services every time even if they’ve had a procedure covered previously under the same insurance.
5. Document everything thoroughly. Thorough documentation is the foundation for all solid medical billing. Providers must comprehensively document the medical necessity of procedures and accurately detail all services provided. Equally important is the role of coders, who must be able to accurately interpret the documentation and be accountable for accuracy. Simplifying processes and using templates can help.
6. Code correctly. With more than 10,000 unique medical codes, it’s no wonder mistakes happen. Hiring experienced medical coders and putting in place systems that include checks and balances can help guarantee their accuracy and avoid financial and legal consequences. According to the Medical Group Management Association (MGMA), reworking a denied claim costs $25 on average , which can quickly add up.
7. Bundle codes when possible. According to the American Medical Association (AMA), unbundling is one of the most common coding mistakes healthcare providers make. Instead of using a separate code for each component of a procedure, a single code that encompasses them all should be used when one is available. While unbundling may lead to larger reimbursements, it can also serve as red flags to auditors, posing risks to your bottom line and reputation in the long run.
8. Eliminate upcoding and undercoding. Both upcoding (inflating reimbursement requests with additional services or more expensive ones) and undercoding (not seeking enough reimbursement) can impact your bottom line, even when unintentional. The former can land you in severe hot water, too. The AMA provides an example of a psychiatrist who billed for more time than he actually met with patients. He was hit with a $400,000 fine and excluded from Medicare and Medicaid.
9. Review denials and rejections. No matter how solid your billing practices are, denials are still inevitable. When a claim is denied, it’s important to understand why. If it’s due to a coding error, incorrect billing information or another oversight, it can be corrected and/or an appeal can be made to gain reimbursement. Many practices don’t take action, however. According to MGMA, 50% to 65% of denials are never worked , which can result in lost revenue.
10. Embrace technology. There are a plethora of advanced solutions today designed to make the medical billing process more efficient and accurate than traditional paper methods. Technologies such as artificial intelligence (AI), predictive analytics and automation can provide insight, help prevent errors, streamline processes and optimize revenue.
Of course, these technologies are also constantly evolving, so staying abreast of the latest trends and developments and regularly evaluating your practice’s needs is essential, as well.

Joseph is a Content Marketing Analyst at LendingTree where he works to empower people to make their best financial decisions. He earned his B.A. from Penn State University.
- Understanding The Challenges and Opportunities For Patients in Telemedicine
- Cost Containment Strategies for Healthcare Organizations in 2024
- How Price Transparency Can Benefit Both Providers and Patients
- 5 Ways to Control Costs During Healthcare Construction Projects
most recent

Strategies for Reducing Data Costs in Healthcare

Enhancing Medical Training Effectiveness: Leveraging Data-Driven Innovations in Medical Education

AI-powered prior authorization: A catalyst for building a more equitable healthcare system

The Adoption of Digital Twin Technology Comes with Cybersecurity Concerns

Hospital Financial Assistance Shouldn’t Be ‘Charity Care’

Strategies to Optimize Time and Reduce Healthcare Burnout with AI
Healthcare Business Today is a leading online publication covering the healthcare industry.
Pittsburgh, PA
© healthcare business today 2024

Answers to the 5 Most Commonly Asked Billing & Coding Questions
Fill form to unlock content.
Error - something went wrong!
Fill out the form to view webinar.

Ronda Tews, CPC, CHC, CCS-P Senior Director, Billing and Coding Compliance, ModMed
This webinar was recorded April 17, 2024.
We understand it can be difficult to keep up with ever-evolving billing and coding regulations and best practices, especially when you have a busy practice to run. But accurate billing is vital to the success of your business, as even the smallest mistakes could result in delayed or lost revenue.
We’re here to help! Join us for this exclusive webinar where Senior Director of Billing and Coding Compliance, Ronda Tews, will address the five most common billing and coding questions our team gets asked throughout the year.
YOU WILL LEARN:
- Medicare guidelines for billing PA- or NP-provided services under a practice physician’s NPI (incident-to-billing)
- Two types of scenarios when billing a physician under another physician is allowed
- Standards for billing for an office-based procedure versus an ambulatory surgery center
- Which place of service to select when billing for nursing home visits
- How to categorize an established patient visit at a new practice (when to use “new patient” versus “established patient”)

Knowing the rules can help practices receive payments that better reflect the work of the whole health care team.
BETSY NICOLETTI, MS, CPC
Fam Pract Manag. 2024;31(3):9-14
Author disclosure: no relevant financial relationships.
Medical services are usually billed by the individual who performs the service. However, Medicare has two exceptions — “incident to” and “shared services.” These two rules essentially allow physicians to bill for care provided by clinicians and staff who work with them as if the physicians had done it themselves. They're similar rules, but with key differences.
Incident-to services are performed in physician offices or patients' homes, while shared services are performed in facilities such as hospitals or nursing homes. Incident-to services can be performed by either non-physician clinicians (NPCs) or clinical staff as part of the billing physician's professional services, while shared services must be performed by two clinicians (physicians or NPCs) who each could have billed the service on their own. (See “ Incident-to vs. shared services comparison .”)
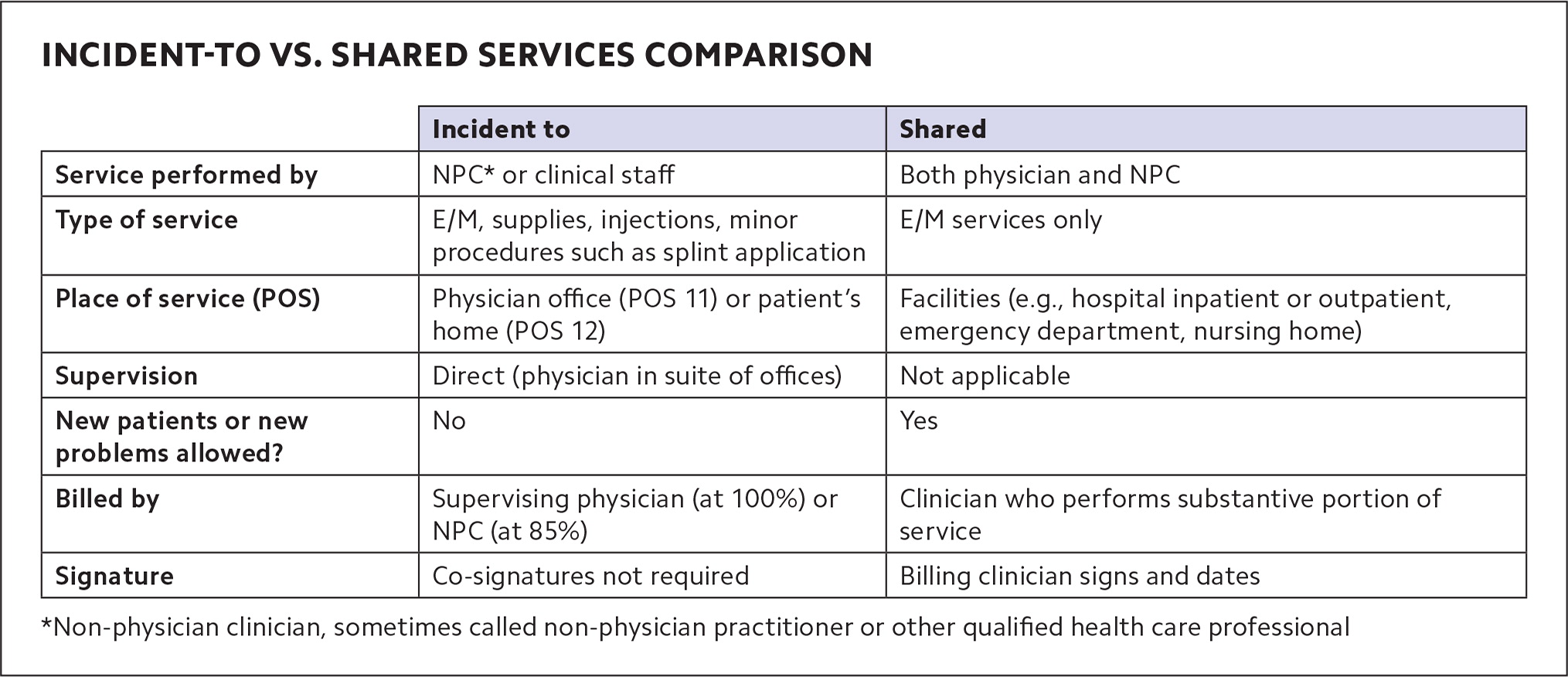
In either case, though, if the physician is billing, Medicare pays the full physician fee schedule rate, while services billed by NPCs are paid at 85% of that. Some private insurers also allow incident-to billing and shared services billing under rules similar to Medicare's, but this varies by payer.
Shared services rules have changed recently, as CPT has published new definitions (which Medicare has largely adopted, for now). The requirements for incident-to billing haven't changed, but they can be confusing, and because family physicians tend to use incident-to billing more often, a refresher is useful. This article provides that refresher on incident-to billing, as well as an explanation of the changes to shared services billing, and has a set of questions and answers with specific scenarios to help physicians understand when and how to use each of them.
Medicare allows supervising physicians to bill for services that other members of the health care team provide in office or home settings (“incident-to” billing) and bill for services they provide jointly with other clinicians in facility settings (“shared services”).
Some private payers also allow incident-to billing and shared services billing, and CPT has released definitions for shared services.
Shared services are billed by the physician or other clinician who performed the “substantive portion” of the E/M visit, which is easier to determine when using total time.
INCIDENT-TO REFRESHER
Incident-to rules allow a supervising physician to report services performed by NPCs or auxiliary clinical staff as if the physician personally provided them. NPCs are most often physician assistants or nurse practitioners. They're sometimes called “other qualified health care professionals” (QHPs)” or “non-physician practitioners” (NPPs), but in this article we'll refer to them as NPCs. Clinical staff are most often medical assistants or nurses, but could include other professionals who work under physicians' supervision (see “ Definitions ”). Billing for incident-to services under the supervising physician's name and National Provider Identifier (NPI) results in the full reimbursement rate.
DEFINITIONS
Non-physician clinicians (NPCs) or non-physician practitioners (NPPs): Physician assistants and a variety of advance practice registered nurses (e.g., clinical nurse specialists, certified nurse midwives, nurse practitioners, and certified registered nurse anesthetists) who are allowed to bill Medicare directly.
Other qualified health care professional: According to CPT, “A physician or other qualified health care professional is an individual who by education, training, licensure/regulation, and facility privileging (when applicable) performs a professional service within his/her scope of practice and independently reports a professional service. These professionals are distinct from clinical staff.” This includes the NPCs/NPPs above, but also other professionals such as physical therapists and clinical social workers.
Clinical staff member: According to CPT , this is “a person who works under the supervision of a physician or other qualified health care professional and who is allowed by law, regulation, and facility policy to perform or assist in the performance of a specified professional service.” This includes medical assistants and nurses.
NPCs may also use incident-to billing for services clinical staff provide under their supervision. As noted, though, Medicare will pay a lesser rate (85% of the physician fee schedule amount) for incident-to services billed using the NPC's name and NPI on the claim form.
Incident-to services include evaluation and management (E/M) and other services and supplies commonly furnished in medical practices, such as applying a splint, doing an injection, or checking blood pressure at a nurse visit. Incident-to billing does not apply to services with their own statutory benefit categories (i.e., groups of services health plans are legally required to cover), including wellness visits, clinical diagnostic tests, and pneumococcal, influenza, and hepatitis B vaccines.
To bill for a service that an NPC performed under the physician's NPI (at the full physician rate), these requirements must be met:
• The service must be part of a physician's plan of care . The physician sees the patient at a prior encounter and establishes the plan of care. After that, the NPC may see the patient as part of the physician's treatment. (If a subsequent E/M service can be performed entirely by clinical staff, rather than an NPC, the supervising physician may still bill for it as an incident-to service at the full physician rate using E/M code 99211 — the lowest level of E/M. Higher level E/M services must be performed by an NPC or physician.) E/M services for new patients, or new problems for existing patients, aren't eligible for incident-to billing because they are not part of the physician's preexisting plan of care. If an NPC provides these services, they must bill for them under their own NPI (at the 85% rate).
• The service requires direct supervision . The physician, or the physician's covering partner, is in the suite of offices (or patient's home) and immediately able to assist if needed when the NPC performs the service. Medicare rules are generally interpreted as requiring the supervising physician to be in the same or a similar specialty as the NPC performing the service, although the Centers for Medicare & Medicaid Services (CMS) doesn't specifically say this. Likewise, CMS does not specifically define supervision beyond the physician being “in the suite of offices,” but some payers interpret it to mean not separated by a set of stairs or elevator.
• The NPC must be an expense to the practice , either employed, leased, or contracted.
• The physician must stay involved in the plan of care , but CMS does not describe exactly what this entails. It could mean alternating visits with the NPC or periodically seeing the patient. Simply signing off on the record alone is less compelling as documentation, and there is no Medicare requirement for co-signature. NPCs can provide documentation that supports incident-to billing by noting in their assessment that the visit was part of the physician's plan of care and that the physician was in the office. But CMS does not specifically require this.
• The NPC must be enrolled in Medicare , whether billing directly or incident to the physician, according to U.S. Department of Health and Human Services guidance. 1
SHARED SERVICES
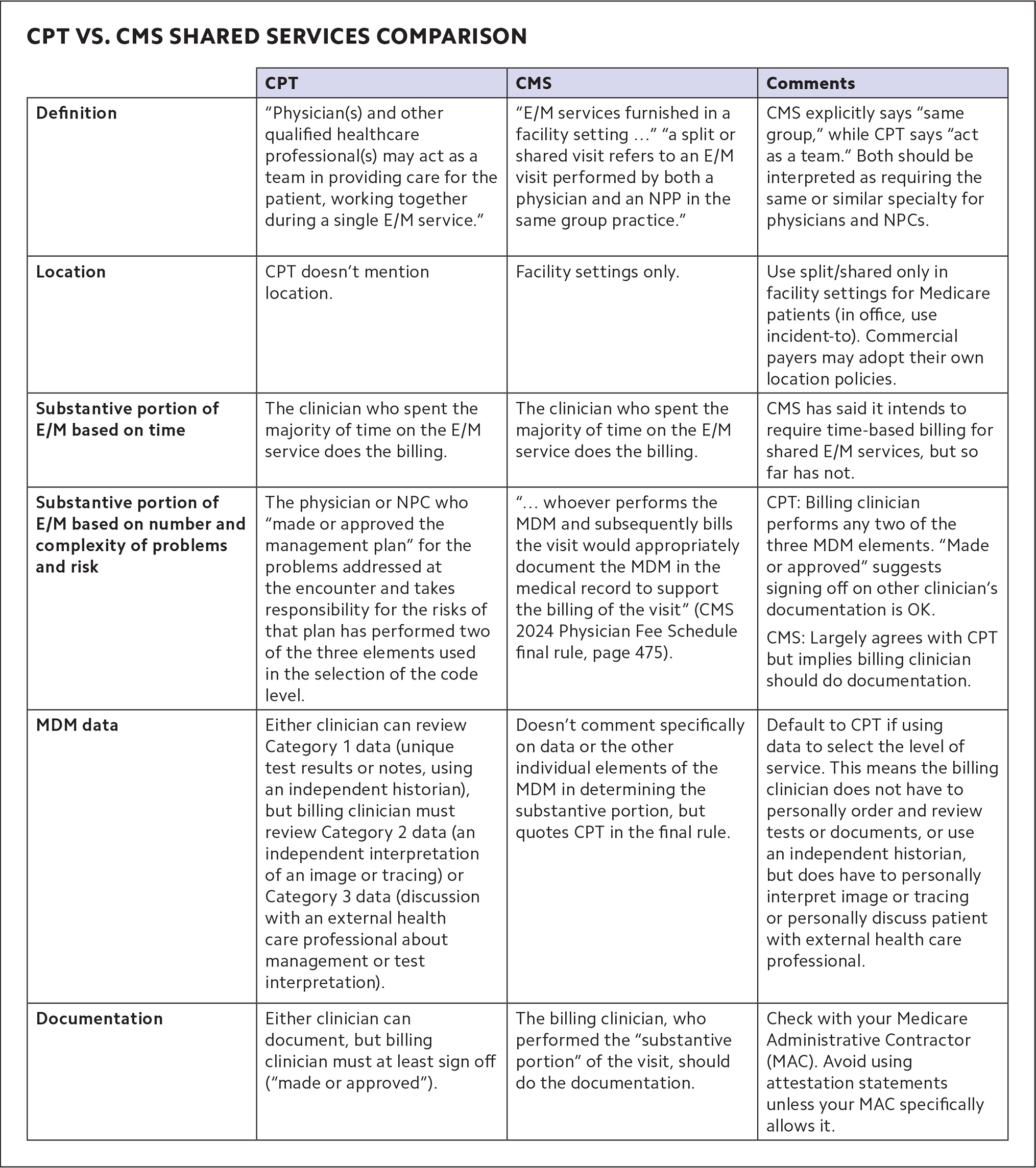
Until recently, only Medicare defined shared services. But CPT added its own definition in 2021 and expanded it in 2024. (See “ CPT vs. CMS shared services comparison .")
Shared services are E/M services that a physician and NPC perform jointly in a facility setting, such as inpatient and outpatient hospital buildings, emergency departments, and nursing homes. Shared services may not be performed in physician offices that are not part of a facility setting. The place of service (POS) code is key to shared services billing. 2 For example, hospital outpatient clinics that use POS 19 (on campus) or 22 (off campus) can bill for shared services, whereas physicians' offices that use POS 11 cannot. (It's the opposite with incident-to services, which can be billed with POS 11, but not POS 19 or 22.)
Both clinicians must be enrolled in Medicare and able to perform E/M services on their own (a physician may not share E/M services with a social worker or dietitian, for example, because those professionals don't have E/M in their scope of practice). 3
To bill for E/M as a shared service, both clinicians must participate in the patient's care on the same calendar day. The identity of both clinicians must be included in the encounter note, but only the billing clinician is required to sign and date the medical record. That clinician then submits the claim using HCPCS modifier FS (“split [or shared] evaluation and management visit”) for Medicare.
Remember that when the physician bills for the shared service, Medicare pays 100% of the physician fee schedule allowance, but when an NPC bills, it results in payment of only 85%. So, it makes sense to bill under the physician's NPI when possible. But under both Medicare and CPT rules, physicians may only do this if they perform the “substantive portion” of the service.
Billing based on time . If you're billing for E/M based on total time, determining who provided the substantive portion of the visit is pretty straightforward: The clinician who accounted for more than half the visit's total time (face-to-face and non-face-to-face time combined) performed the substantive portion of the service. Thus, both clinicians should document their own time, and if the physician's time is greater than half, the service should be billed under the physician's NPI. The only complicating factor with time-based coding is that if the physician and other clinician meet to discuss the patient, or see the patient together, only one of them can count those minutes — they can't double-count them.
Billing based on MDM . If you're using medical decision making (MDM) to code an E/M service, determining who performed the substantive portion is significantly more complicated. There's no quick and clear way to do it, but here is some guidance based on both CPT and CMS rules.
MDM is defined by three elements: the number and complexity of problems addressed, the amount and/or complexity of data reviewed and analyzed, and the risk of morbidity and/or mortality from additional diagnostic testing or treatment. In 2024, CPT added this instruction: “performance of a substantive part of the MDM requires that the physician(s) or other QHP(s) who made or approved the management plan for the number and complexity of problems addressed at the encounter take responsibility for that plan with its inherent risk of complications and/or morbidity or mortality of patient management. By doing so, a physician or other QHP has performed two of the three elements used in the selection of the code level based on MDM. If a practice codes the visit based on medical decision-making (MDM), the practitioner who performs the problems addressed and risk portions of the visit reports the service.” 4
The key takeaways are this:
The physician or NPC who evaluates the problems and determines and takes on the risk of the additional testing and treatment of those problems (two of the three MDM elements) meets the “substantive portion” threshold to qualify as the billing clinician.
CPT states that the billing clinician “made or approved the management plan.” It does not state that the billing clinician must personally document the plan.
There is one twist. If you use data to select the level of E/M service and include Category 2 data (an independent interpretation of an image or tracing) or Category 3 data (discussion with an external health care professional about management or test interpretation), the billing clinician must perform that portion of the service. 4 Category 1 data (ordering and/or reviewing unique test results, reviewing notes, or using an independent historian) does not need to be performed by the billing clinician because this work is included in the formulation of the diagnosis and plan.
Because of the complicated nature of determining who should be the billing clinician using MDM, CMS has said that in the future it intends to require that clinicians only use time to determine who performed the substantive portion of shared services. But CMS delayed that change for the third year in a row in its 2024 Physician Fee Schedule final rule, instead saying it would follow the new CPT definition for now.
CMS also said this about shared services: “Although we continue to believe there can be instances where MDM is not easily attributed to a single physician or NPP when the work is shared, we expect that whoever performs the MDM and subsequently bills the visit would appropriately document the MDM in the medical record to support the billing of the visit.” 5
CMS does not explicitly say what the billing physician needs to document and what the NPP (or NPC) could document instead. Therefore, although CPT's guidance seems to indicate that an attestation statement is acceptable (“made or approved the management plan”), it would be prudent for physicians to personally document MDM when billing Medicare for shared services under their NPI.
PAYMENTS THAT BETTER REFLECT THE WHOLE HEALTH CARE TEAM
Clearly, the rules governing incident-to billing and shared services billing are not always simple. But the list of questions and answers should help clarify some common scenarios.
Having a basic understanding of when shared services and incident-to rules apply allows physicians to receive payments that better reflect the actual work their practices are doing, especially as team-based care increases.
Q: Dr. Taylor sees a patient for hypertension and sets a plan for the patient to return to see the nurse practitioner (NP) to titrate the medication in two weeks. When the patient comes back to see the NP, Dr. Taylor is out of the office, but her partner Dr. Jackson is in the office. Do we bill this latest visit under Dr. Taylor or Dr. Jackson?
A: Dr. Jackson. Bill under the supervising physician who is in the office and able to provide assistance if needed.
Q: A physician sees an established patient for an acute problem, a sprained ankle. Six months later, the patient slips and re-sprains the ankle and the practice's physician assistant (PA) sees the patient. Can the physician bill this as an incident-to service?
A: No, this acute condition is a new problem and should be billed by the PA.
Q: Can you bill incident to if using time to determine the level of evaluation and management?
A: Yes. You can bill incident to if using time or medical decision making.
Q: If a physician and an advance practice registered nurse (APRN) are billing for a shared service E/M visit based on time, do each of them need to document their time?
A: Yes. The clinician who accounted for more than 50% of the time bills for the service, so both the physician and the APRN must document their time. (They can't double-count time if they both see the patient together or meet to discuss the patient.)
Q: Working in an outpatient hospital department, a physician and PA each perform part of an office/other outpatient visit. It is follow up for an urgent care visit over the weekend. The patient has an acute, uncomplicated condition, and a prescription medicine is given for cough control. The physician personally interprets the chest x-ray from the urgent care visit. Under the shared services rules, who should report the E/M service and what is the correct level of service?
A: Two of the three medical decision-making elements are moderate: amount and complexity of data (independent interpretation) and risk (prescription drug management). It is, therefore, a level-4 E/M visit. The physician performed the independent interpretation of data and, therefore, may bill for the visit.
Q: Can we bill for shared services for nursing facility visits?
A: Yes. Skilled nursing visits that use place of service 31 qualify because that is considered a facility location. But nursing facility services in place of service 32 (mostly rehab providers) do not because that is considered a non-facility location. Also, shared services may not be performed for visits mandated to be done by a physician.
Advanced practice registered nurses, anesthesiologist assistants, and physician assistants. Centers for Medicare & Medicaid Services (CMS) Medicare Learning Network. MLN901623; March 2022.
Place of service code set. CMS. Updated September 2023. Accessed March 13, 2024. https://www.cms.gov/medicare/coding-billing/place-of-service-codes/code-sets
Medicare Claims Processing Manual, Ch. 12, Sec. 30.6.18A. CMS 100-04; rev. 12461. Jan. 18, 2024. Accessed March 14, 2024. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf
CPT 2024 Professional Edition . American Medical Association; 2023.
CMS-1784-F. CMS. Nov. 16, 2023. Accessed March 14, 2024. https://www.cms.gov/medicare/medicare-fee-service-payment/physicianfeesched/pfs-federal-regulation-notices/cms-1784-f
Continue Reading
More in FPM
More in pubmed.
Copyright © 2024 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
An example of a 99204 or 99214 is a patient being seen for follow-up of hypertension and diabetes, which are well-controlled. ... prolonged visit codes can be used. The AMA CPT committee developed ...
The E/M visit CPT® codes 99202-99215 (new and established patients) were revised to decrease documentation and ... Follow-up as needed. Medical decision-making for this case is a straightforward review of a single self -limiting problem, with review of minimal data and a minimal level of risk;
Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making. When using time for code selection, 30-39 minutes of total time is spent on the date of the encounter. About the CPT code set.
The codes apply to services that a wide range of primary care and specialty providers perform regularly. Some of the most commonly reported E/M codes are 99201-99215, which represent office or other outpatient visits. In 2020, the E/M codes for office and outpatient visits include patient history, clinical examination, and medical decision ...
CPT® code 99213: Established patient office or other outpatient visit, 20-29 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...
Coders can gain insight into follow-up evaluation and management (E/M) billing patterns and potential coding risks by reviewing the episode of care, or the sequence of managed care events for a patient's presenting problem. For example, a coder reviews an internal medicine provider's progress note. A summary of relevant documentation states ...
Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter. 99204. Office or other outpatient visit for the ...
(Follow-Up Care) CPT Codes 99291 & 99292 When you provide the entire initial critical care service and report CPT code 99291, any provider in the same . specialty and the same group providing care concurrently to the same patient on the same date should report . their time using the code for additional time intervals (CPT code 99292).
• Reach out to patients as soon as you are notified of their ED visit to schedule their follow-up visit. Follow-up care for people with mental health conditions can result in fewer repeat ED visits, as well as improved physical and mental function, and increased compliance with follow-up instructions. • Receiving timely information from ...
99495 Transitional Care Management Services with the following required elements: Communication (direct contact, telephone, electronic) with the patient and/or caregiver within 2 business days of discharge. Medical decision making of at least moderate complexity during the service period. Face-to-face visit, within 14 calendar days of discharge.
October 1, 2017 Reporting Follow‐Up Encounters Q. How do I report an encounter for a follow‐up visit when the condition has been resolved? A. Per the ICD‐10‐CM guidelines "Do not code conditions that were previously treated and no longer exist." "The follow‐up codes (Z08, Z09, Z39) are used to explain continuing surveillance
CPT code 99233 is assigned to a level 3 hospital subsequent care (follow up) note. 99233 is the highest level of non-critical care daily progress note. When it comes to 99233 documentation is critical, however understanding of the documentation required is even more critical. WorK RVU (wRVU) for cpt code 99233 is of course higher than that for ...
The basic format of codes with levels of E/M services based on medical decision making (MDM) or time is the same. First, a unique code number is listed. Second, the place and/or type of service is specified (eg, office or other outpatient visit). Third, the content of the service is defined. Fourth, time is specified.
Coding Reference Guide Measurement Year 2024 Follow-Up After ED Visit for People with Multiple High-Risk Chronic Conditions (FMC) ... Seven-Day Follow-Up Visits (including visits that occur on the date of the ED visit) Outpatient Visit, Telephone Visit, E-Visit or Virtual Check-In ... Case Management Visits CPT: 99366 HCPCS: T1016, T1017, T2022 ...
Although, "there are some notable differences in this area when it pertains to CPT® versus CMS," Jimenez forewarned. "One of the biggest changes, I think, in the 2023 changes was the elimination of observation codes," Jimenez said. Effective Jan. 1, 2023, hospital observation codes 99217-99220 and 99224-99226 are deleted.
The changes to 2021 Evaluation and Management (E/M) coding involve only outpatient codes for new patient visits and follow-up visits described by Current Procedural Terminology (CPT) codes 99202-99205 and 99211-99215. 1 Knowing the history of the development of these codes and the rationale for the code changes is key to understanding the ...
According to the Medical Group Management Association (MGMA), reworking a denied claim costs $25 on average, which can quickly add up. 7. Bundle codes when possible. According to the American Medical Association (AMA), unbundling is one of the most common coding mistakes healthcare providers make. Instead of using a separate code for each ...
This webinar was recorded April 17, 2024. We understand it can be difficult to keep up with ever-evolving billing and coding regulations and best practices, especially when you have a busy practice to run. But accurate billing is vital to the success of your business, as even the smallest mistakes could result in delayed or lost revenue.
If the insurers list differs from that recommended by the AAP, report the insurer to the AAP, which will follow up on your behalf. Some practices have trouble with reimbursement on a three- or four-day visit for newborns discharged 24 hours after birth. In this case, it is recommended that you use office-visit codes 99212-99215 for this three ...
Yes, it's possible to have both Medicare and Medicaid if you qualify. People who have both Medicare and full Medicaid coverage are "dually eligible.". Medicare pays first when you're dually eligible and you get Medicare-covered services. Medicaid pays last, after Medicare and any other health insurance you have.
Scheduled follow-up visit for multiple significant but stable problems. Remember to show extra work to justify 99214 vs. 99213. ... Medicare does not cover CPT codes 99381-99397, because Medicare ...
Note, the testing code includes the time spent talking with the patient about the risks and benefits of treatment and/or waiting for the test results. Subsequent visit billing: When your ENT sees the patient for a follow-up visit to check the patch test results, you cannot report this encounter with additional units of 95044. Reading the ...
The place of service (POS) code is key to shared services billing. 2 For example, hospital outpatient clinics that use POS 19 (on campus) or 22 (off campus) can bill for shared services, whereas ...